 WASHINGTON, DC — The idea for VA’s Close To Me Infusion Service has its roots in many places, One of them a veteran that Jenna Shields, PharmD, BCOP, saw weekly at the Pittsburgh VAMC. Suffering from a hematologic condition, he required weekly infusions that could only be given at the medical center. To make that weekly appointment, he awoke at 3:30 a.m. to catch a bus from a remote community-based outpatient clinic (CBOC) to the hospital, where he would arrive before most doctors.
WASHINGTON, DC — The idea for VA’s Close To Me Infusion Service has its roots in many places, One of them a veteran that Jenna Shields, PharmD, BCOP, saw weekly at the Pittsburgh VAMC. Suffering from a hematologic condition, he required weekly infusions that could only be given at the medical center. To make that weekly appointment, he awoke at 3:30 a.m. to catch a bus from a remote community-based outpatient clinic (CBOC) to the hospital, where he would arrive before most doctors.
This veteran would wait hours for the lab to open so he could get his monthly blood tests. Then the new infusion dose would be calculated, the pharmacist would make it and he would receive it. The infusion procedure itself took only five minutes to complete. Then he would get on the bus for the long ride back home.
 “He was on a treatment that you received weekly. Indefinitely. There was no endpoint to this treatment,” declared Shields, who had been working as an oncology clinical pharmacy specialist at the Pittsburgh VA at the time. “This guy was lovely. He never complained. I was complaining for him… Why does he have to do this?”
“He was on a treatment that you received weekly. Indefinitely. There was no endpoint to this treatment,” declared Shields, who had been working as an oncology clinical pharmacy specialist at the Pittsburgh VA at the time. “This guy was lovely. He never complained. I was complaining for him… Why does he have to do this?”
Shields and her colleagues started examining whether the veteran could get his infusions at the CBOC near his home rather than the medical center.
“We developed a policy and procedure,” Shields explained. “We worked with the pharmacy to figure out how we were going to transport the infusion to the CBOC. We traveled to the clinic and trained the nurses how to assess the patient and administer the treatment. Then we set up the process for the patient to see us [at the Pittsburgh VAMC] monthly to set up his dosage for the rest of the month.”
The result was the veteran needing to make the trip to Pittsburgh once a month rather than once a week, reclaiming whole days that had previously been lost to travel and waiting.
While this might have been the seed, it would be the Minneapolis VA Healthcare System that did the first full pilot, bringing infusion services to 16 CBOCs in the Minneapolis catchment area and showing that what Shields and her colleagues did for this one veteran could be scaled larger.
The end result was Close To Me, which is working to bring cancer care–and care for other diseases that require infusion–closer to veterans’ homes. It also led to Shields becoming VA’s National Oncology Program Pharmacy Manager.
 Infusion treatment can be a laborious process. After a veteran is diagnosed and infusion treatment is prescribed, patients get pre-clearance tests that can take weeks. Then the day of their first treatment they might have multiple education sessions with nurses and pharmacists before even going to the infusion room.
Infusion treatment can be a laborious process. After a veteran is diagnosed and infusion treatment is prescribed, patients get pre-clearance tests that can take weeks. Then the day of their first treatment they might have multiple education sessions with nurses and pharmacists before even going to the infusion room.
For some, the treatment might take a handful of minutes. For chemotherapy, it can take hours.
“Currently, most of the infusion rooms are located in urban VAs. They’re often landlocked and there can be terrible traffic and parking. It’s not always an enjoyable experience,” Shields noted. “Because a lot of times veterans are traveling a long way they’re trying to consolidate their appointments into one day. They’re seeing docs, getting labs, getting treatment, getting meds. It’s a full day at the clinic experience. And then everyone is trying to get out before rush hour.”
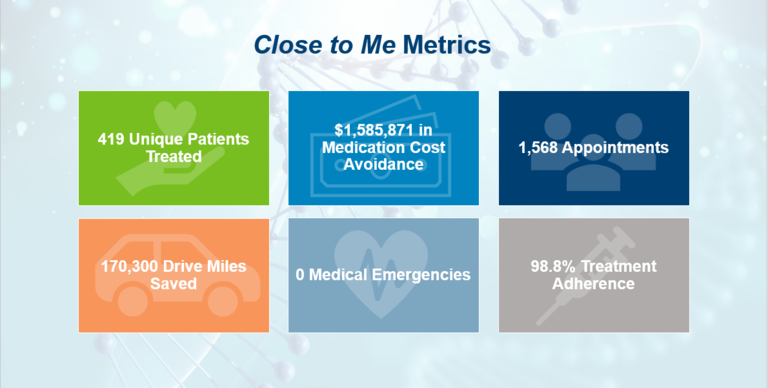
The benefit of a nearby infusion service isn’t just seen in hours recovered for patients, but in treatment success. Veterans who have to travel may not be able to keep up with the full treatment regimen, skipping whole days or weeks because of difficulty getting to the infusion site. Data from the program shows closer infusion sites are cutting no-shows in half.
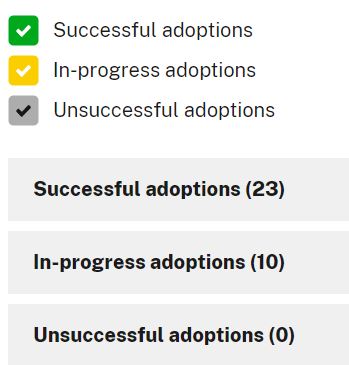
To date, Close To Me has helped four medical centers expand infusion services to their CBOCs with eight more soon to come. But Shields would like to see this service become standard for VA oncology programs.
“There are about 130-odd VAs that have oncology programs and I would like to see every program be able to provide infusions throughout their CBOC catchment area eventually,” she said.
In the long-term that means VA needs to start thinking about infusion services when they’re designing and constructing new clinics.
“We’re currently utilizing buildings that were meant for primary care and making that work for now,” she said. “It’s not just oncology that needs this. Other specialties provide infusion, too.”
Shields also wants to see the program provide more direct provider-to-patient care.
“Close To Me in its original iteration is sending nursing teams out to CBOCs to give infusions while using telehealth for the providers,” she explained. “We’re looking now at putting advance practice providers into some of the CBOCs to actually provide the infusion care.”
Because the program is, by its very purpose, targeting more remote areas, hiring will be one of the biggest challenges.
“Sending traveling teams from the main hub hasn’t been that challenging to staff…but as we look at expansion it will get harder to find experienced oncology providers,” Shields said.
Close To Me is also looking at two models for at-home infusion care, as well as utilizing mobile units. Those models are still in development and have yet to be fielded.
In the meantime, Shields and others are looking at what hospitals Close To Me can assist next, focusing on those with rural veteran populations who have the greatest travel burden.
“I grew up in rural Kansas,” Shields explained. “My family lived about two hours from Kansas City and I saw my grandparents as they were aging refuse to drive to the city to receive the care that I thought that they needed… I understand the burden of travel and how under-resourced these communities are becoming. That’s something really close to my heart.”

