ATLANTA — Colorectal cancer (CRC) remains a major health threat in the United States, ranking as the fourth most common cancer among men and women combined. Each year, approximately 156,000 Americans receive a CRC diagnosis, and more than 50,000 die from the disease. The lifetime risk of developing CRC is about one in 24 for men and one in 26 for women, with an average diagnosis age of 66.1
Once primarily seen in older adults, in recent years the incidence of CRC has risen substantially in younger individuals. One in five diagnoses now occurs in people in their early 50s or younger, twice the rate seen in 1995, prompting revision of screening recommendations to begin at age 45.2
The VA diagnoses approximately 4,000 new CRC cases annually, accounting for about 9% of all cancer cases among veterans, making it an area of keen interest.3,4 While veterans tend to be older and overweight or obese, have more comorbidities and are more likely to have a history of smoking, which all increase the risk of developing CRC, they also have some unique risk factors.
For military personnel and veterans, exposure to environmental hazards connected to deployments increases the likelihood of developing serious health conditions, including CRC. One of the most pressing concerns in recent years has been burn pits, which have been associated with multiple types of cancer.
Recognizing these risks, The Sergeant First Class Heath Robinson Honoring our Promise to Address Comprehensive Toxics Act of 2022 (PACT Act) designates all gastrointestinal cancers, including CRC, as presumptive conditions for veterans exposed to burn pits, ensuring access to VA healthcare and disability benefits without requiring proof of direct service connection. To be eligible for PACT Act compensation for exposure to burn pits or other toxins, veterans must have served at some point since Aug. 2, 1990, on the ground or in the airspace above Bahrain, Iraq, Kuwait, Oman, Qatar, Saudi Arabia, Somalia, United Arab Emirates, the Arabian Sea, the Gulf of Aden, the Gulf of Oman, the neutral zone between Iraq and Saudi Arabia, the Persian Gulf or the Red Sea; or since Sept. 11, 2001, on the ground or in the airspace above Afghanistan, Djibouti, Egypt, Jordan, Lebanon, Syria, Uzbekistan or Yemen.5
In addition to burn pit exposure, chronic infections such as hepatitis B and C, which are more prevalent among veterans, increases CRC risk.6 Chronic inflammation from these infections can lead to DNA damage, increasing susceptibility to malignancies. Many veterans who served overseas may have been unknowingly exposed to viral infections that elevate their long-term cancer risk, making consistent screenings even more critical.
VA Efforts to Combat CRC
Ensuring that all veterans, especially those at increased risk, receive timely screenings is a priority for the VA. A number of programs including reminders in the electronic health system and mailed fecal immunochemical tests to veterans with average risk of CRC have successfully increased screening rates among veterans, which significantly exceed that seen in non-veterans, 78.44% for veterans vs. 68.62% in the broader U.S. population.4
“Our analysis of one of the largest national health surveys shows that U.S. veterans are more likely to be screened endoscopically for CRC than the rest of the general population, which is concordant with other studies which have shown similar findings,” said Aasma Shaukat, a gastroenterologist with the N.Y. Harbor VAMC, and her colleagues in an article in Gastroenterology & Endoscopy. “This is due in part to the higher likelihood of veterans having healthcare coverage through the Veteran Affairs (VA) health benefits program, compared to non-veterans.”
“The increased proportion of screening in this patient population and the higher utilization of colonoscopies in veterans compared to other modalities, lines up with findings from studies utilizing the national VA-Medicare database which show a substantial reduction in CRC mortality in veterans,” Shaukat and colleagues added.
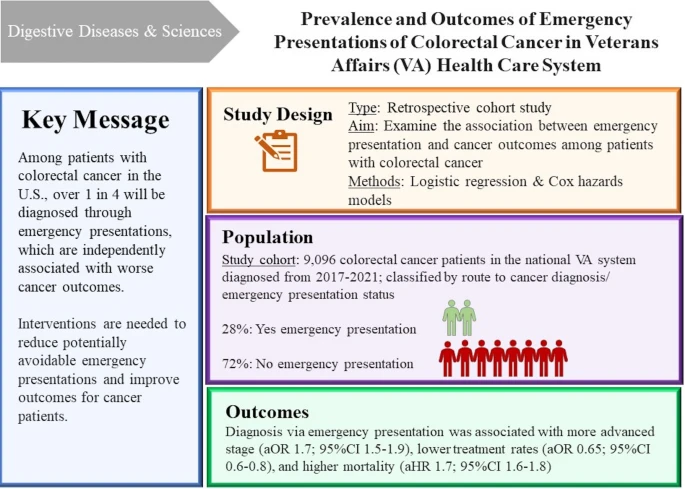
Still, more than 28% of veterans with CRC were first diagnosed because they presented to the emergency department with symptoms. These veterans were 70% more likely to have advanced disease, 35% less likely to receive treatment for CRC and 70% more likely to die of the malignancy, a recent study led by a team at the Michael E. DeBakey VAMC found.7
“While the increased mortality risk seen in our study was in part attributable to more advanced stage at diagnosis and lower treatment rates, we found that even when these and other important factors were accounted for, [emergency presentations] remained an independent predictor of overall mortality among patients with CRC,” the DeBakey team found.
Tailoring treatment for veterans with metastatic CRC
Between 15% and 30% of CRC cases present initially with metastatic disease; an additional 20% to 50% of patients diagnosed with local disease will eventually develop metastases.8
To improve treatment outcomes among veterans with metastatic CRC, the VA’s National Precision Oncology Program (NPOP) makes molecular testing available to guide personalized treatment plans and offers discussions about tumor test results with members of the Molecular Oncology Tumor Board. Pharmacogenomic testing further helps physicians select the most appropriate medications and dosages for treatment. Veterans may also participate in clinical trials offering access to the latest therapies based on the genomic profile of their tumors.9
The VA’s ongoing efforts in cancer research and treatment accessibility through all stages of CRC will play a crucial role in improving outcomes among veterans with this common cancer. Ensuring all veterans benefit from these innovations will be vital in the years ahead.
- American Cancer Society. Colorectal Cancer Facts & Figures 2023-2025. Atlanta: American Cancer Society Inc. 2022.
- Siegel RL, Wagle NS, Cercek A, Smith RA, Jemal A. Colorectal cancer statistics, 2020. CA: A Cancer Journal for Clinicians. 2023 Mar 1;73(3):233-254.
- U.S. Department of Veterans Affairs. VHA 2024 Annual Report: VA Health Care: A Strong Foundation. A Healthy Future.
- Adenusi AO, Obaitan I, Monteiro JFG, Asifat O, Shaukat A. Endoscopic and stool-based colorectal cancer screening coverage among US veterans: A survey analysis using 2021 Behavioral Risk Factor Surveillance System (BRFSS) data. Gastroenterology & Endoscopy. 2024;2(4):181-185.
- H.R.3967—Honoring our PACT Act of 2022. Congress.gov.
- Kaur A, Azeez GA, Thirunagari M, et al. Association of Chronic Hepatitis B With Colorectal Cancer and Its Dual Impact on Colorectal Liver Metastasis: A Narrative Review. Cureus. 2024 Dec 20;16(12):e76079.
- Khalaf N, Ali B, Zimolzak AJ, et al. Prevalence and Outcomes of Emergency Presentations of Colorectal Cancer in Veterans Affairs Health Care System. Dig Dis Sci. 2025 Jan;70:177–190. Epub 2024 Dec 11.
- Cervantes A, Adam R, Roselló S, Arnold D, Normanno N, Taïeb J, Seligmann J, De Baere T, Osterlund P, Yoshino T, Martinelli E; ESMO Guidelines Committee. Metastatic colorectal cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol. 2023 Jan;34(1):10-32. doi: 10.1016/j.annonc.2022.10.003. Epub 2022 Oct 25.
- VA National Precision Oncology Program. What Is VA’s National Precision Oncology Program (NPOP)?