BOSTON—Venetoclax combinations are common treatments for individuals with acute myeloid leukemia (AML) who are unable to withstand the rigors of intensive induction chemotherapy. While results with these combinations have been encouraging in clinical studies, real-world outcomes have been markedly worse.
A team of investigators from the VA Boston Healthcare System and other medical institutions in Boston sought to determine whether preexisting psychiatric diagnoses and substance-use disorders—not typically seen in clinical trial participants—would affect results of venetoclax treatments in veterans with AML.
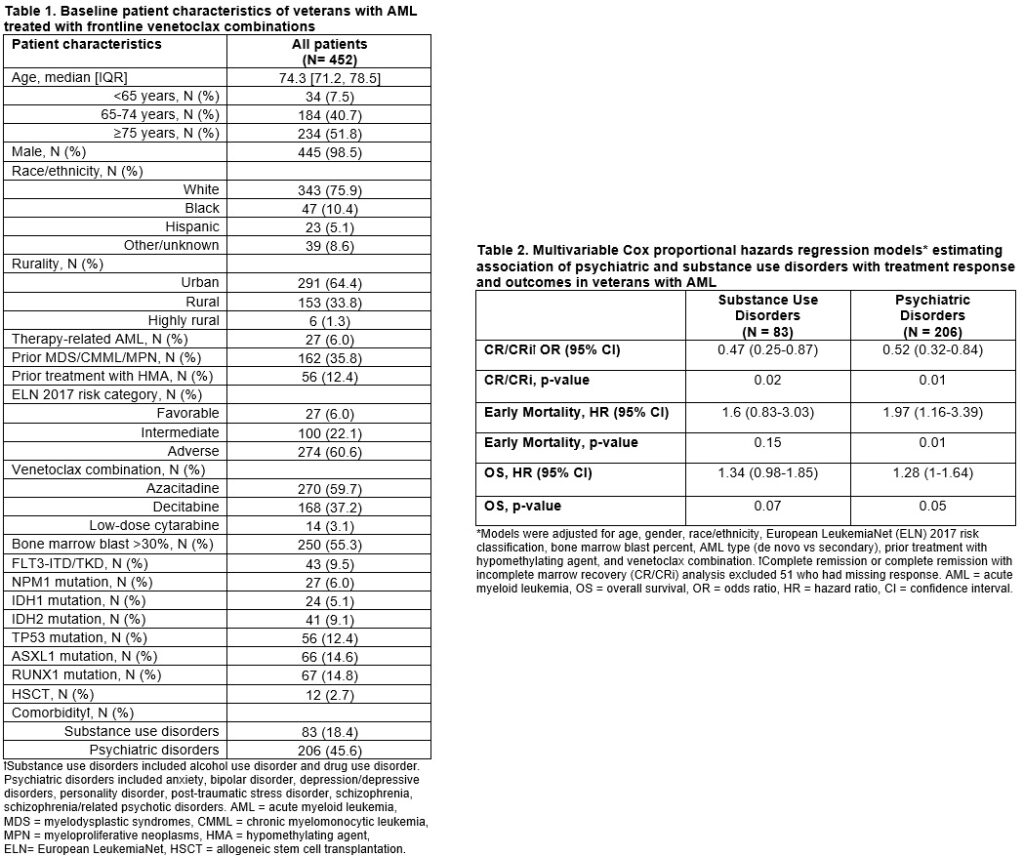
In a study of 452 veterans with AML treated with the combinations, the researchers found that the majority had preexisting diagnoses of psychiatric issues or substance disorders. Further, these diagnoses significantly negatively impacted outcomes, the team said in a presentation at the 65th American Society of Hematology Annual Meeting in San Diego in December 2023.1
Of the treated veterans, 97% received venetoclax with either azacitidine (60%) or decitabine (37%), and 3% received venetoclax with low-dose cytarabine.
Lee MH, La J, Brophy MT, Do NV, Edwards CV, Dumontier C, Hobbs GS, Fillmore NR. Psychiatric and Substance Use Disorders Are Independent Predictors of Treatment Response and Outcomes in United States Veterans with Newly Diagnosed Acute Myeloid Leukemia Treated with Venetoclax Combinations. Abstract 388. ASH 2023. December 9, 2023.
Forty-six percent of the veterans had a psychiatric diagnosis, and 19% had a substance-use disorder (SUD), while 11% had both. Among veterans younger than age 65, 68% had psychiatric disorders compared to 50% of those 65 to 74 years old and 39% of those aged 75 and older. Likewise, the proportion of those with substance-use disorder decreased as age increased, with 38% of those under age 65, 26% of those 65 to 74, and 9% of those age 75 or older having a SUD.
Still, the majority of veterans, 57%, experienced either complete remission (CR) or complete remission with incomplete marrow recovery (CRi), and 3% proceeded to allogeneic stem cell transplantation (SCT). Of those who received SCT, none had a substance-use disorder, and eight had a psychiatric diagnosis. Median overall survival was 216 days (95% CI: 195-254). The 60-day mortality rate of 20% included eight veterans who developed primary refractory AML.
Notably, veterans with SUD had more than twice the rate of admissions to intensive care as those who did not, at 5% and 2.2% per five person-years. Multivariable analyses found that both psychiatric diagnoses and SUDs independently decreased the odds of complete remission or complete remission with incomplete marrow recovery. In addition, veterans with psychiatric disorders had nearly twice the risk of early mortality (95% CI: 1.16-3.39, p=0.01) and a 1.28 times higher hazard of death (95% CI: 1.00-1.64, p=0.05) when compared to those with psychiatric diagnoses.
The researchers suggested that “veterans with psychiatric and SUDs may have difficulty adhering to regimens, reemergence of their mental instability and illness that is triggered by AML diagnosis and its treatment, or biologic mechanisms associated with these comorbidities.” Consideration of interventions that provide additional support to veterans with AML and concurrent psychiatric or substance-use disorders may improve outcomes, they noted.
1Lee MH, La J, Brophy MT, Do NV, Edwards CV, Dumontier C, Hobbs GS, Fillmore NR. Psychiatric and Substance Use Disorders Are Independent Predictors of Treatment Response and Outcomes in United States Veterans with Newly Diagnosed Acute Myeloid Leukemia Treated with Venetoclax Combinations. Abstract 388. ASH 2023. December 9, 2023.

