AUSTIN, TEXAS — Veterans who develop age-related macular degeneration (AMD) now have a variety of treatments available that can preserve and even improve vision—and more are on the way. In wet AMD, the options are exploding, while VA research has also identified a possible treatment for dry AMD.
While laser therapy and photodynamic therapy are sometimes used to treat wet or neovascular AMD, the most common treatment relies on injections of anti-vascular endothelial growth factor (VEGF) drugs into the eye. These drugs slow or stop the growth of the abnormal blood vessels behind the retina characteristic of wet AMD, and reduce the leakage of those that have developed. Anti-VEGF injections are the most common eye procedure in the world, and more than 10 million people in the U.S. receive the treatments each year.
“Veterans with an aggressive form of AMD called ‘exudative’ or ‘wet’ may benefit from medications injected into the eye or laser treatment to reduce swelling and leakage inside the eye,” VA Spokesperson Gina Jackson told U.S. Medicine. “Studies have shown that these medications can improve visual outcomes and reduce scarring for at least seven years. Durable, longer-lasting, medications are emerging that may reduce the frequency of injections needed for macular degeneration.” Medications requiring fewer appointments and injections promise several advantages.
While anti-VEGF treatments have proved remarkably effective in clinical trials, protecting vision in up to 90% of participants, real-world data shows about a much lower 50% success rate. The lower rate is attributed to poor patient adherence to recommended injection schedules and obstacles to care such as finding transportation to appointments.
Those issues can be particularly acute for veterans. Nearly one-quarter of all veterans live in rural communities, which tend to have fewer specialists of all kinds. The greater distance to a VAMC or retinal specialist can be especially problematic for veterans with vision loss who may not be able to drive themselves. In addition, more than 55% of rural veterans are over age 65 and are more likely to have multiple medical conditions that make traveling to appointments particularly burdensome.
Advances in Anti-VEGF Treatment
Seven anti-VEGF drugs have received U.S. Food and Drug Administration approval for use in wet AMD. Ranibizumab (Lucentis) and ranibizumab-nuna (Byooviz) typically require monthly injections for at least the first year. Pegaptanib sodium (Macugen) is injected every six weeks, although it has largely been displaced by other agents. Aflibercept (Eylea) can be administered every eight weeks after a three-month start-up period of monthly injections. Brolucizumab (Beovu) was granted FDA approval in 2019 for administration every eight to 12 weeks after three monthly injections to start.
Bevacizumab (Avastin), which is approved for cancer treatment, is also used off-label for AMD and typically requires monthly injections. The VA specifically restricts bevacizumab use to hematology/oncology applications in its national formulary.
The FDA granted approval to a new delivery system for ranibizumab, Susvimo, which uses a refillable ocular implant to reduce the number of injections required, while providing comparable benefits to monthly injections. The device delivers ranibizumab continuously and needs to be refilled about every six months. The implant, roughly the size of a grain of rice, is inserted during a one-time outpatient procedure. Patients may receive additional injections while using the device, if needed. The Velodrome study currently underway is evaluating the efficacy of Susvimo refilled every nine months instead of six.
Retired navy veteran William Chicky received a Susvimo implant after his diagnosis with wet AMD, at a point where he could not read the big E on the eye chart. “It really is pretty devastating finding out your eyesight is going down the tube and how long it’s going to be before you go blind you don’t know,” he told CBS Austin. Chicky received monthly injections until he received the implant, then needed just one refill in 2021. With treatment, his eyesight went from legally blind to 20/25 vision.
In late January, another drug with a new mechanism of action received FDA approval. The bispecific antibody Faricimab (Vabysmo) not only blocks VEGFs, like the other approved drugs for wet AMD, it also blocks angiopoietin-2, which weakens blood vessels and makes them more likely to break or leak. Faricimab is administered in four monthly loading doses then every eight, 12 or 16 weeks, based on the patient’s optical coherence tomography (OCT) and visual acuity, for a year.
In the identical Phase 3 Tenaya and Lucerne trials, nearly half of the 1,329 participants went 16 weeks between doses, while another third spaced their doses 12 weeks apart.1 The researchers found faricimab non-inferior to aflibercept in efficacy and the drugs had comparable rates of ocular adverse events. Overall, they found “visual benefits with faricimab given at up to 16-week intervals demonstrate its potential to meaningfully extend the time between treatment with sustained efficacy, thereby reducing treatment burden in patients with nAMD.”
Treatments in the Pipeline
For some patients, treatment spacing could be much longer. Researchers at Johns Hopkins Medicine said that up to one-third of patients receiving anti-VEGF therapies could safely stop treatment, though not before biomarkers identifying the best candidates are developed. Individuals who could halt treatment without fluid accumulation in the eye or vision loss produce different levels of specific proteins in their retinal fluid, they found.2
New treatments in development include retinal gene therapy, in which an adeno-associated virus carrying therapy that encourages the retina to produce its own VEGF-A blocking proteins is injected in the eye or inserted in a surgical procedure. Gene therapy, if effective, could offer a permanent solution to the disorder. Four drug candidates are being evaluated for wet AMD treatment and one for dry AMD.
VA researchers from the South Carolina Columbia VA Health Care System with support from its affiliated nonprofit Dorn Research Institute working with a team at the University of Virginia School of Medicine discovered that medications used in human immunodeficiency virus (HIV) prevention, nucleoside reverse transcriptase inhibitors, may substantially reduce the risk of dry AMD. Their study of 33 million patients over a 20-year period revealed that individuals taking the HIV drugs had a 40% lower likelihood of developing dry AMD.
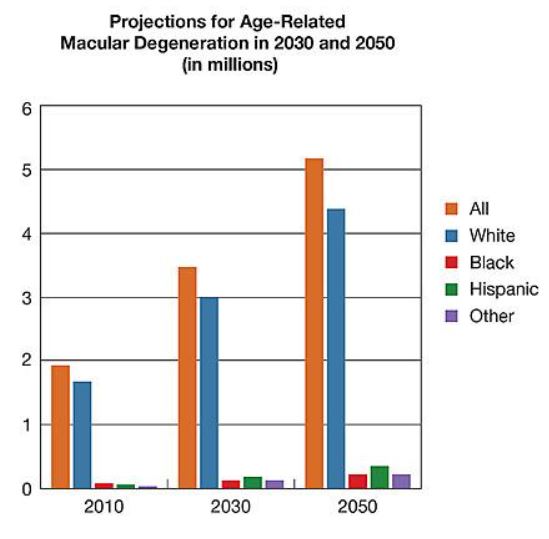
“The database results back genetic findings from the study that explain how the HIV drugs might help protect vision,” said VA Investigator Scott Sutton, PharmD, a clinical researcher at the Dorn Research Institute and South Carolina Columbia VAMC and chair of the Department of Clinical Pharmacy at the University of South Carolina College of Pharmacy. “The results are intriguing and offer promise for a new approach to preventing and treating a disease that affects millions of veterans and non-veterans.”
- Heier JS, Khanani AM, Quezada Ruiz C, Basu K, Ferrone PJ, Brittain C, Figueroa MS, Lin H, Holz FG, Patel V, Lai TYY, Silverman D, Regillo C, Swaminathan B, Viola F, Cheung CMG, Wong TY; TENAYA and LUCERNE Investigators. Efficacy, durability, and safety of intravitreal faricimab up to every 16 weeks for neovascular age-related macular degeneration (TENAYA and LUCERNE): two randomised, double-masked, phase 3, non-inferiority trials. Lancet. 2022 Jan 21:S0140-6736(22)00010-1. doi: 10.1016/S0140-6736(22)00010-1. Epub ahead of print. PMID: 35085502.
- Cao X, Sanchez JC, Dinabandhu A, Guo C, Patel TP, Yang Z, Hu MW, Chen L, Wang Y, Malik D, Jee K, Daoud YJ, Handa JT, Zhang H, Qian J, Montaner S, Sodhi A. Aqueous proteins help predict the response of patients with neovascular age-related macular degeneration to anti-VEGF therapy. J Clin Invest. 2022 Jan 18;132(2):e144469. doi: 10.1172/JCI144469. PMID: 34874918; PMCID: PMC8759792.