Early Onset CRC Has Different Clinical Features
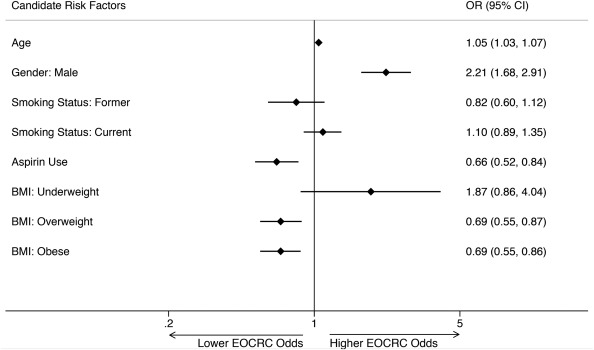
Click to Enlarge: Early-onset colorectal cancer risk factors. Results of a multivariable model estimating odds for EOCRC with candidate risk factors is depicted. ∗Denotes statistical significance where P < .05. All variables listed in the figure met forward stepwise selection criteria (P < .05) and were included in the multivariable regression model. Variables selected out of the model include (1) race/ethnicity and (2) diabetes. Hosmer-Lemeshow goodness-of-fit P value = 0.6. Source: Journal Gastroenterology
ROCHESTER, MN — Colorectal cancer (CRC) is the third-most-common cancer globally and ranks second as the most-common cause of cancer-related mortality. Until recent decades, it was viewed as primarily a disease of the elderly, with average occurrence in their late 60s for men and early 70s for women.
What has puzzled researchers and clinicians in recent decades, however, is the troubling increase in the incidence of CRC in adults younger than age 50 in the United States and in other high-income countries. A study last year in the New England Journal of Medicine last year pointed out that early-onset CRC now makes up about 10% of new cases of the cancer. An increase in mortality of younger patients has accompanied the rising trend.1
The American Cancer Society reported that, among older adults, cancer death rates continued to decline 0.6% in those 50 to 64 and 2.6% in those 65 and older from 2013-2017, although not as rapidly as from 2004-2013, when the rates were 1% and 3.3%, respectively.
On the other hand, CRC death rates have increased in individuals younger than 50 years of age by 1.3% per year, since 2004.
“The concurrent increase in early-onset colorectal cancer and decline in later-onset cases have shifted the median age at diagnosis from 72 years in the early 2000s to 66 years at present,” according to the NEJM review from the Mayo Clinic’s Frank A. Sinicrope, MD. “In the next 10 years, it is estimated that 25% of rectal cancers and 10 to 12% of colon cancers will be diagnosed in persons younger than 50 years of age.”
Projections are that early-onset colorectal cancer will double in younger patients, who often present with more advanced disease because of delayed diagnosis.
Because of recommendations lowering the age of screening from 50 to 45, the Military Health System will have 200,000 additional beneficiaries who need to undergo testing, according to Chin Hee Kim, MD, deputy chief of specialty care support of the DHA Directorate of Medical Affairs.
Interestingly, colorectal cancer in younger patients appears to have different clinical features than later-onset disease. “Early-onset colorectal cancers are most commonly detected in the rectum, followed by the distal colon; more than 70% of early-onset colorectal cancers are in the left colon at presentation,” the NEJM article advised. “By comparison, later-onset colorectal cancers (those diagnosed in patients ≥50 years of age) occur at similar frequencies in the proximal colon and distal colorectum.”
The VA has played a key role in researching early onset colorectal cancer. A study in 2020 noted that the reasons for rising EOCRC incidence and mortality continued to be perplexing. “Some have hypothesized that the rising trend may be related to common or increasingly prevalent modifiable behaviors, such as excess body weight, low physical activity, and diabetes mellitus,” wrote the authors from the University of California San Diego, the VA San Diego Healthcare System and colleagues. “Additionally, non-modifiable risk factors such as race/ethnicity may be associated with EOCRC compared to later-onset CRC”
With results published in the journal Gastroenterology, the researchers conducted a case-control study of U.S. veterans 18 to 49 years old who underwent colonoscopy examinations from 1999 through 2014. The study team identified EOCRC cases from a national cancer registry, while cancer-free veterans, determined by baseline colonoscopy through three years of follow-up, made up the control group.2
Data on age, sex, race/ethnicity, body weight, body mass index (BMI), diabetes, smoking status and aspirin use were collected for the study which, for final analysis, included 651 EOCRC cases and 67,416 controls. Median age of participants was 45.3 years, and 82.3% were male.
Results indicated that a higher proportion of cases were older, male, current smokers, nonaspirin users who had lower BMIs, compared with the controls. In adjusted analyses, the researchers determined that increasing age and male sex were significantly associated with increased risk of EOCRC, but aspirin use and being overweight or obese (relative to normal BMI) were significantly associated with decreased odds of EOCRC.
Weight Loss Early Sign
“In post hoc analyses, weight loss of 5 kg or more within the 5-year period preceding colonoscopy was associated with higher odds of EOCRC (odds ratio 2.23; 95% CI 1.76-2.83),” they explained, adding, “Weight loss may be an early clinical sign of EOCRC. More-intense efforts are required to identify the factors that cause EOCRC and signs that can be used to identify individuals at highest risk.”
Researchers from the Rocky Mountain Regional VAMC were involved in the development of new guidelines by the international Delphi Initiative for Early-Onset Colorectal Cancer (DIRECt).
“Patients with early-onset colorectal cancer (eoCRC) are managed according to guidelines that are not age-specific. A multidisciplinary international group (DIRECt), composed of 69 experts, was convened to develop the first evidence-based consensus recommendations for eoCRC,” according to a report in Clinical Gastroenterology & Hematology.3
The DIRECt group produced 31 statements in seven areas of interest:
- diagnosis,
- risk factors,
- genetics,
- pathology-oncology,
- endoscopy,
- therapy and
- supportive care.
The panel reported a strong consensus that all individuals younger than 50 should undergo CRC risk stratification and prompt symptom assessment. In addition, it emphasized that all newly diagnosed eoCRC patients should receive germline genetic testing and that is best to occur before surgery. “On the basis of current evidence, endoscopic, surgical, and oncologic treatment of eoCRC should not differ from later-onset CRC, except for individuals with pathogenic or likely pathogenic germline variants,” the guideline authors wrote. “The evidence on chemotherapy is not sufficient to recommend changes to established therapeutic protocols. Fertility preservation and sexual health are important to address in eoCRC survivors. The DIRECt group highlighted areas with knowledge gaps that should be prioritized in future research efforts, including age at first screening for the general population, use of fecal immunochemical tests, chemotherapy, endoscopic therapy, and post-treatment surveillance for eoCRC patients.”
- Sinicrope FA. Increasing Incidence of Early-Onset Colorectal Cancer. N Engl J Med. 2022 Apr 21;386(16):1547-1558. doi: 10.1056/NEJMra2200869. PMID: 35443109.
- Low EE, Demb J, Liu L, Earles A, Bustamante R, Williams CD, Provenzale D, Kaltenbach T, Gawron AJ, Martinez ME, Gupta S. Risk Factors for Early-Onset Colorectal Cancer. Gastroenterology. 2020 Aug;159(2):492-501.e7. doi: 10.1053/j.gastro.2020.01.004. Epub 2020 Jan 9. PMID: 31926997; PMCID: PMC7343609.
- Cavestro GM, Mannucci A, Balaguer F, Hampel H, et. al.; Collaborative Group of the Americas on Inherited Gastrointestinal Cancer; European Hereditary Tumour Group, and the International Society for Gastrointestinal Hereditary Tumours. Delphi Initiative for Early-Onset Colorectal Cancer (DIRECt) International Management Guidelines. Clin Gastroenterol Hepatol. 2022 Dec 20:S1542-3565(22)01171-5. doi: 10.1016/j.cgh.2022.12.006. Epub ahead of print. PMID: 36549470.

