Test Everyone?

Navy Veteran Patrick McGuire, a Stage 4 cancer survivor, was one of the first participants of the PHASeR testing
at the Durham, NC, VA Health Care System. Testing was made possible, thanks to a $25 million gift from
philanthropist Denny Sanford with a matching donation from Sanford Health. —VA photo by Ashleigh Barry
“If you were to test everyone, it would be more efficient up front,” said Deepak Voora, MD, director of VA’s Pharmacogenomics Action for Cancer Survivorship, or PHASeR, program. “The challenge is knowing who would be getting those medications and not testing people who would never take the drug. An intermediate approach might be, when testing for one drug that will be prescribed in the next week or so, testing for all drugs to avoid reincurring the testing costs.”
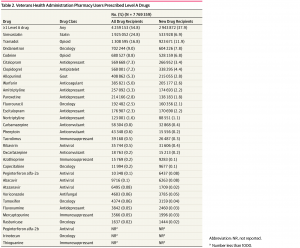
The VA has started to take this approach with certain patient groups. Through a partnership announced in March with Sanford Health Care of Sioux Falls, South Dakota, the PHASeR program provides pharmacogenetic testing for veterans who are cancer survivors. Research shows cancer survivors have a high risk of chronic mental health, metabolic disease and chronic pain. The program will preemptively test for mutations in genes associated with drugs used to treat these conditions, explained Voora.
The PRecision medicine In MEntal health Care, or PRIME Care, study is evaluating the utility of pharmacogenetic testing in veterans with major depressive disorder. Six of the top level A drugs are antidepressants. Using genetic information to guide selection and dosing could dramatically reduce the time spent trying to find an effective medication, as antidepressants are typically given a trial of about six weeks and many patients must try several.
For wider use, Chanfreau-Coffinier recommended more research to determine when to conduct testing. “The optimal timing of testing is still unknown, and more data is needed to evaluate whether a reactive approach (e.g., testing at the time the drug is ordered) or a preemptive approach is preferable,” she said.
Complicating the issue, both the number of genetic variants known to impact drug safety and efficacy and the number of drugs affected by those variants continues to grow.
“While the genetic information provided by pharmacogenomic (PGx) testing does not change over time, its interpretation regarding the list of drugs impacted and the clinical actions recommended is a domain evolving rapidly,” Chanfreau-Coffinier told U.S. Medicine.
Keeping test results accessible over a veteran’s lifetime creates another potential sticking point.
“Pharmacogenetic testing is very different from most tests physicians use,” Oslin said. “Most tests have a very, very short half-life of utility, while these are relevant for a long period of time. To make them relevant to me as a prescriber, I need the information when I am prescribing. We need to marry the data to prescribing behavior.”
Continue Reading: