CHICAGO — Giving more active feedback to primary care pharmacists about their heart failure patients led to more interactions and a greater number of medication adjustments, according to a presentation at a recent conference.
The late-breaking research, The PHARM-HF A&F Study, was presented at the American Heart Association’s Scientific Sessions 2024, held in mid-November in Chicago. The study involved 120 VHA primary care pharmacists responsible for the care of 7,224 veterans with heart failure under the care of 337 primary care teams.
Patients were a median age of 75, and 98% were men. Most of the participants, 65%, were white adults, while 14% were Black adults, 5% were Asian adults, 1% were Native American or Alaska Native people, 4% were Pacific Islander adults, and race was unknown for 11%. As self-identified, 86% of the participants were non-Hispanic, 8% as Hispanic and, for 6%, ethnicity was unknown.
As part of the study, researchers from Stanford University and the VA Palo Alto, CA, healthcare system and colleagues gave the pharmacists educational resources and feedback about the care they were providing to heart failure patients, to assess whether this could improve patient care by improving heart failure medication treatment.
Primary care pharmacists in VA healthcare are embedded within primary care panels and work closely with primary care physicians and nurses on medication management for patients.
“In the VHA, primary care pharmacists can provide medication counseling, necessary monitoring, and they can independently prescribe indicated therapies,” explained lead study author Alexander Tarlochan Singh Sandhu, MD, MS, a cardiologist specializing in heart failure at Stanford University in Palo Alto, CA. “They are empowered to identify individuals who would benefit from guideline-recommended treatments that are not being prescribed, such as heart failure medical therapy, and permitted to contact the patients to initiate therapy.”
During the study evaluation period between January and May 2024, the primary care pharmacists were randomly assigned to one of three study groups:
- the control group, who received educational materials about treatment protocols, monthly webinars and a database of frequently asked questions about heart failure management;
- an audit and feedback group, who received educational materials and monthly audit and feedback emails nudging heart failure medication management; and
- a third group of pharmacists who received educational materials, monthly audit and feedback emails, plus targeted information listing patients with heart failure who had potential for improvement with their medication regimen.
Of 120 primary care pharmacists, 28 were randomized to AF (audit and feedback), 30 to AF+ (audit and feedback with targeted patient information), and 62 to usual care (UC).
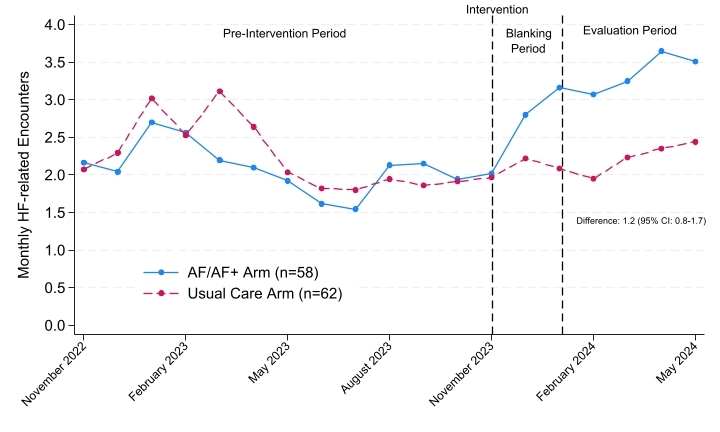
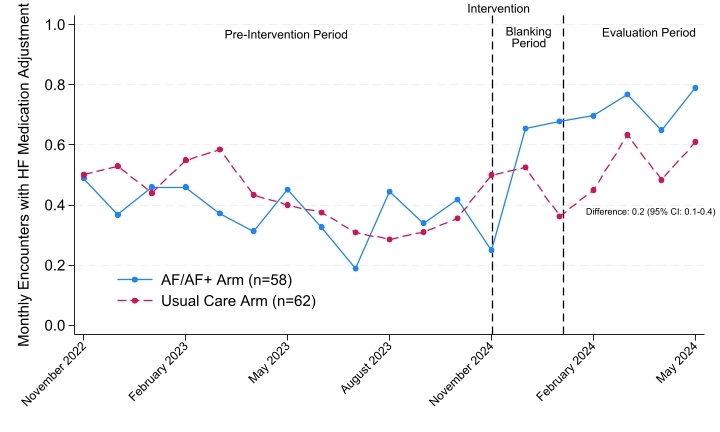
Before the study period, according to the report, each pharmacist averaged two patient visits per month that included heart failure care and 0.4 patient visits per month that included an adjustment of heart failure medication. The primary endpoint of the study was the difference in the rate of HF medication adjustment encounters between the combined AF/AF+ arms and UC during the post-blanking evaluation period 3-6 months post-randomization. Secondary endpoints were the number of HF patients treated, and the percentage prescribed to each class of HF therapy.
“Pre-intervention, each pharmacist averaged 2.1 encounters per month related to HF and 0.4 encounters with HF medication adjustment,” the authors explained. “During the evaluation period, between January 2024 and May 2024, pharmacists randomized to AF/AF+ had 1.2 (95% CI: 0.8-1.7, p<0.01) additional monthly HF encounters and 0.2 (95% CI: 0.1-0.4, p=0.01) additional encounters with HF medication adjustment (Figures 1-2). There were no significant differences between AF and AF+ arms.”
They added that HF patients in clinics with AF/AF+ pharmacists were more likely to receive new mineralocorticoid receptor antagonist prescriptions (11.3% vs. 9.0%; p=0.01), but there were no other significant differences in HF medication prescriptions. Mineralocorticoid receptor antagonist is the most under-prescribed component of heart failure medication therapy, according to the researchers.
“Pharmacists who were audited and received feedback had an additional significant increase in the frequency in which they managed heart failure patients, with 1.2 more visits with patients per month and more heart failure medication adjustments, with 0.2 more visits per month compared with the education-only arm,” the study team noted. “However, adding access to patient-specific information in addition to the audits and feedback did not result in any improved outcomes.”
Sandhu pointed out, “We found that when pharmacists participated in the audit and feedback group, they were more likely to identify patients who would benefit from medication adjustment, set up new appointments with patients to adjust heart failure medications and adjust heart failure medication therapy during appointments, thus potentially leading to improved heart failure management and better patient outcomes.”
“This shows one approach to increasing the use of pharmacists to improve heart failure medication use, and it may also be applicable to other chronic diseases,” he added. “This is a major opportunity to improve health for more patients, especially in a system like the Veterans Affairs Healthcare System with a large, robust network of pharmacists nationwide.”
Sandhu advised that a strength of this study was its practical approach and that it is an intervention that is highly scalable but said a major limitation was that the patient-specific data provided to pharmacists was not restricted to their own roster of patients.
“The main surprise was that patient-specific data did not lead to an additional increase in heart failure medication adjustment,” he suggested. “We know pharmacists can help improve medical therapy for patients with heart failure, however, most pharmacists are not providing heart failure care even when they are allowed to.”
- Sandhu AT, Steverson AB, Sahy A, Gholami, et. Al. Evaluation of Randomized Audit and Feedback to Increase Heart Failure Medication Optimization Among Primary Care Pharmacists in the Veterans Affairs Health Care System (PHARM-HF A&F Study). Presented at American Heart Association’s Scientific Sessions 2024, Chicago, IL, Nov. 16-18. Abstract Number 4168636.