NASHVILLE, TN — For healthcare systems changing over from one electronic health record (EHR) system to another—such as the VA’s transition from its legacy EHR system to Oracle Cerner EHR modernization program—the transition poses many challenges, including an impact on medication safety.
Despite the implementation of bar-code medication administration (BCMA) technology, which has successfully reduced errors to some extent, medication administration is a time-intensive nursing task prone to errors. One analysis of sentinel events found that errors in medication administration were linked to the EHR’s medication administration record (MAR) specifically designed for BCMA. Additionally, documented instances of BCMA workarounds, such as bypassing medication or patient armband scans, highlight the challenges that arise when the intended workflows clash with the realities of nursing practice.
A new study published in the Journal of General Internal Medicine examines how one medical center enlisted nurses to identify potential BCMA problems with nurses’ transition among EHR systems. Insights from the study could have implications for any healthcare system undergoing an ERH system transition.1
In the study, researchers at Vanderbilt University Medical Center (VUMC) employed simulation-based comparative usability testing of BCMA tasks to assess progress during the transition from a legacy EHR system to a commercially available EHR product. With the support of the nursing team, from executive nurse leaders to the bedside nurses, researchers selected study tasks based on nursing team input, existing new nurse training, and previously known BCMA challenges, said Carrie Reale, MSN, senior quality assurance analyst at VUMC’s Center of Research and Innovation in Systems Safety. “We created realistic scenarios and then allowed nurses to complete tasks independently as if they were doing the actual work.”
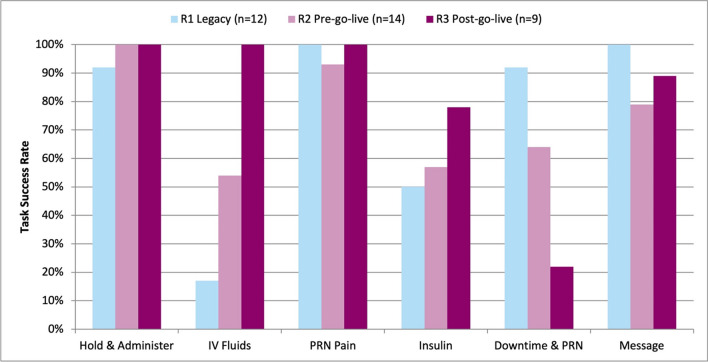
The evaluation included three rounds of data collection: legacy system baseline performance, preliminary end-user performance in the new system prior to go-live and follow-up evaluation 4 months post-implementation in the new system.
Fifteen staff nurses with varying levels of nursing experience completed 2- to 3-hour simulation sessions. Practice settings included adult and pediatric patient populations in ICU, step down and acute-care departments. Tasks included hold/administer, IV fluids, PRN pain, insulin, downtime/PRN and messaging. The researchers systemically analyzed audiovisual recordings of task performance for time, navigation and errors and interviewed nurses post-simulation to gather qualitative comments and perceptions of the system.
Although interviews revealed a largely positive attitude toward the EHR transition, analysis of the qualitative data uncovered three major usability themes expressed by nurses: increased documentation burden, excessive alerts/prompts and inefficient flowsheet design.
“We expected to uncover some usability issues when nurses first used the new system,” said Reale. “More interesting was that, even with use of a well-established EHR by experienced nurses, poor user interface design elements continued to contribute to errors and increased workload.”
In most cases, nurses performed better on the post-implementation tasks compared to pre-implementation and legacy performance, the researchers found. Except for Downtime/PRN and Message tasks, success rates were maintained or improved post-implementation compared to baseline.
The IV fluids and insulin tasks saw the highest combined average error rates across rounds. Overall error rates generally decreased with the intervention. Specifically, the nurses who completed all three rounds demonstrated a 50% reduction in safety-related errors during the post-implementation tasks compared to pre-implementation, and 53% compared to legacy system performance.
“By identifying specific areas of difficulty and patterns of use errors, we were able to make practical recommendations to the EHR implementation team to help mitigate these risks prior to go-live,” said Reale. “This helped set appropriate expectations for nursing workload changes and increased confidence in the transition process.”
In addition to the insight the study provided for VUMC, it also “demonstrated that usability testing with clinicians can be effectively incorporated into EHR transition roadmaps without causing delays or derailing resources and interdependent timelines,” Reale said. “This effort yielded pragmatic, evidence-based insights to guide transition planning, target end user training, and prioritize future EHR build enhancements.
“We strongly recommend healthcare organizations and EHR vendors incorporate targeted usability evaluation into their transition and ongoing monitoring strategies to increase EHR safety, efficiency, effectiveness, and end-user satisfaction.”
- Reale, C., Ariosto, D. A., Weinger, M. B., & Anders, S. (2023). Medication Safety Amid Technological Change: Usability Evaluation to Inform Inpatient Nurses’ Electronic Health Record System Transition. Journal of general internal medicine, 38(Suppl 4), 982–990. https://doi.org/10.1007/s11606-023-08278-1