SAN ANTONIO — Even with the availability of monoclonal antibody medications, VA patients with primary refractory or relapsed large B-cell lymphoma (LBCL) have poor outcomes.
The standard of care for those veterans is salvage therapy (ST) as second-line treatment, according to a presentation at the recent 64th Annual ASH Meeting and Exposition in New Orleans. The next step could be high-dose therapy with autologous stem cell transplant (ASCT) in chemo-sensitive patients; only about 30-40% of stem cell transplant are considered eligible to undergo transplant, it noted.1
The study led by researchers from the South Texas Veterans Health Care System and the University of Texas Health San Antonio MD Anderson Cancer Center, both in San Antonio, pointed out that chimeric antigen receptor (CAR) T-cell therapy is the current standard of care for high-risk LBCL (high International Prognostic Index (IPI), HIT status) who do not respond to ST and have manageable safety profiles and high efficacy. “Promising CAR T data is also emerging for early chemotherapy failure and as alternative second-line therapy,” the authors explained.
The goal of the study was to analyze the treatment patterns and survival outcomes of veterans with primary refractory and relapsed population of LBCL within the VHA.
The retrospective chart review of 5,199 randomly selected patients with an ICD code for lymphoma treated within the VHA involved the period between Jan. 1, 2011, and Dec. 31, 2019. Included were patients with LBCL who completed first-line chemotherapy treatment and had documented post-treatment scans (PET, CT). Primary refractory status was defined as either stable disease (SD) or progressive disease (PD) based on post-treatment scans and relapsed disease as recurrence of disease within 12 months of post-treatment scans, according to the researchers. Ultimately, 2,288 patients who received or completed treatment at the VHA met inclusion data.
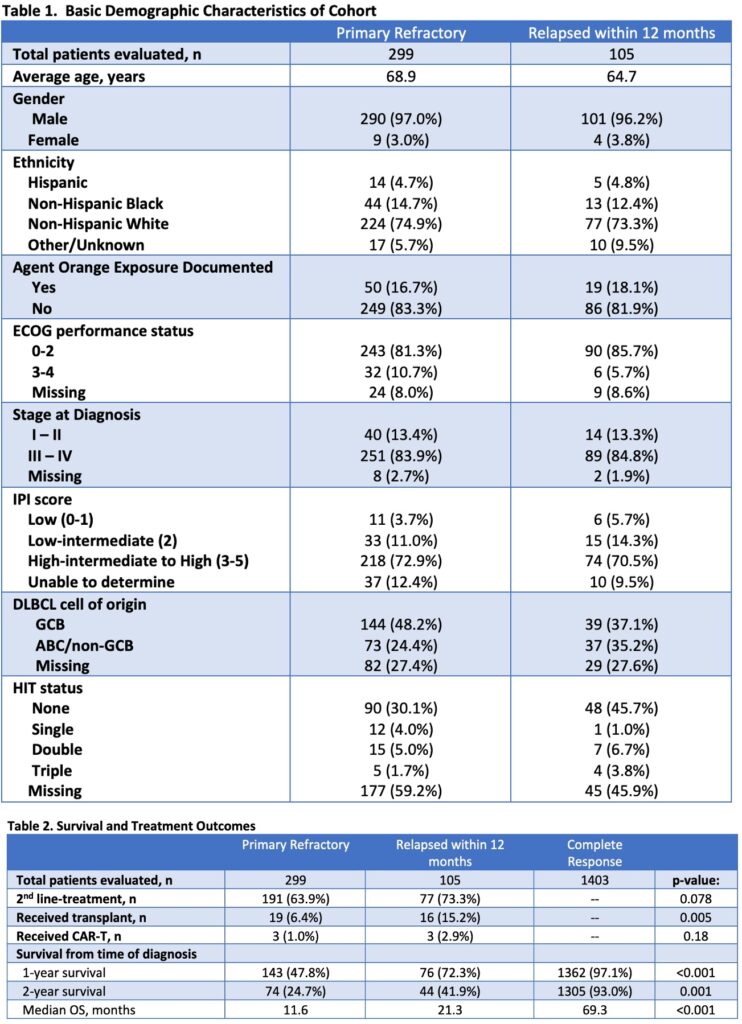
From the study team’s analysis, 299 (13.1%) of patients were primary refractory. The median age of those veterans was 68.9 years, and 97% were male. European Cooperative Oncology Group (ECOG) was 0-2 (81.3%). Stage at diagnosis was III-IV (83.9%), with most patients, 85%, having an IPI score of 3 or more.
The researchers reported that germinal center B-Cell (GCB) accounted for 48.2%, while Activated B-Cell (ABC) was 24.4%. They determined gene rearrangement in 26% of the patients with available data.
Of the 63.9% of patients who received second-line treatment, only 6.4% were able to receive high dose chemotherapy and underwent an ASCT, and only 1% of patients received CAR T-cell therapy. Results indicated that one-year overall survival was 47.8%, with two-year overall survival at 24.7%, respectively. Median OS for the veteran cohort was 11.0 months.
The study also noted that the cohort had 4.6% relapsed patients. Of those, median age was 64.7 years, and 96.2% were male. ECOG was 0-2 (85.7%), while stage at diagnosis was III-IV at 84.8%. Most of those patients, 80%, had an IPI score of 3 or greater. Germinal center B-cell-like (GBC) subtype accounted for 37.1%, while activated B cell (ABC) was 35.2%. In addition, gene rearrangement was present for 20% of the patients with available data. Only 15.2% of patients received high-dose chemotherapy and ASCT, and only 2.9% received CAR T-cell therapy. For them, one- year and two-year overall survival was 72% and 41%, respectively, with median OS at 21.3 months.
Overall, 61% of the veterans had complete response (CR) with a one- and two-year survival rate of 97 % and 93 %, respectively, and median OS of 69.3 months.
“This is one of largest data sets studying the rate of primary refractory and relapsed LBCL in the VHA and shows that more than two-thirds of these patients have high-risk disease,” the authors wrote. “Furthermore, a significant portion of these veterans did not receive second-line therapy including ASCT as compared to previously reported real world and clinical trial data.”
The researchers posited that the patient populations might have had higher rates of chemo resistance, were deemed ineligible for transplant due to age or performance status or had higher rates of comorbidities. “Emerging data on newer antibodies and CAR T-cell therapy for early chemotherapy failure or second-line therapy might be a more appropriate option for our veteran population,” they explained. “In conclusion, CAR T-Cell therapy will likely replace the treatment paradigm for primary refractory or relapsed disease for early treatment failures in patients with LBCL.”
- Boyle LD, Kaur S, Souza GR, Ananth S, et. al. Survival Outcomes for High Risk Primary Refractory and Relapsed Large B-Cell Lymphoma (LBCL) within the Veterans Health Administration (VHA). Presented at the 64th Annual ASH Meeting and Exposition; December 2022; New Orleans, LA.