WASHINGTON, DC — After years of improvements, severe staffing shortages are back on the rise at VA. According to a VA Office of the Inspector General (OIG) report released last month, fiscal year 2022 put an end to a three-year staffing improvement, with facilities reporting 2,622 severe occupational staffing shortages spread across 256 occupations. This is compared to 2,152 reported in FY 2021.
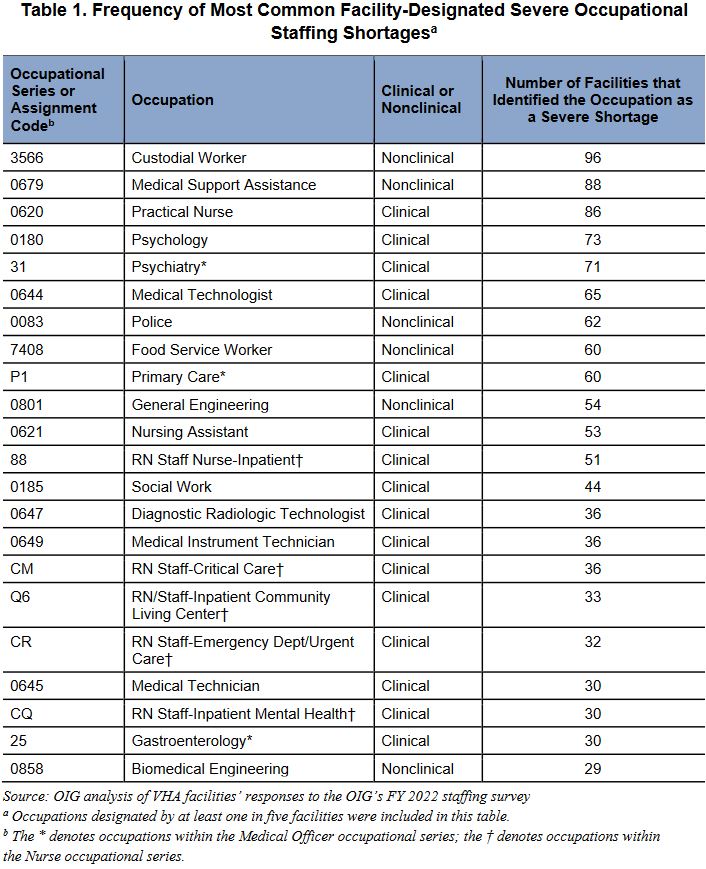
Some of these shortages are in occupations that historically have been hard to fill, including nurses and medical officers, which is a category that includes primary care physicians and medical specialists. However, for the first time since the department updated its reporting requirements in 2017, nonclinical occupations took the top spots on the list. This year also marks the first time that facilities reported more than 90 occupations with severe shortages.
According to the report, 91% of VA facilities reported severe shortages among nurses, and 87% reported severe shortages among medical officers. Among the physician positions with the highest reported shortages are psychiatry, primary care and gastroenterology. The most common nurse shortages include practical nurses, as well as resident nurses for inpatient care, community living centers, urgent care and inpatient mental health.
Taking the top two spots on the list are custodial worker and medical support assistance. In FY 2022, 69% of facilities reported a severe custodial worker shortage, up from 42% in FY 2021. Although medical support assistance came in second on the list, it continues a three-year trend of shortages in that profession, increasing from 36% in FY 2020 to 62% in FY 2021 to 88% in FY 2022.
While the medical community has been predicting an increasingly dire healthcare worker shortage for years, the pandemic has accelerated that shortage, especially for nurses and support workers.
A study released by Mayo Clinic researchers in December 2021 found that about half of physicians and support personnel reported feeling burned out from the pandemic, a number that rose to 63% for nurses. Many reported experiencing high stress, fear of exposure, anxiety, depression and a high workload. When asked if they felt valued by their organizations, nurses had one of the lowest ratings at 30%. One third of medical support personnel reported intending to leave in the near future, as did 40% of nurses surveyed.
In May 2022, Surgeon General Vivek Murthy, MD, released an advisory calling for healthcare facilities to immediately address the issue of worker burnout, noting that researchers are projecting a shortage of more than three million low-wage healthcare workers in the next five years and a projected shortage of nearly 140,000 physicians by 2033.
“Even before the COVID-19 pandemic, healthcare workers were facing challenges,” Murthy said. “Fifty-four percent of doctors and nurses were already experiencing burnout. With the pandemic, things have gotten worse. … Health workers are leaving their jobs in large numbers. We’re looking at a future without enough doctors, nurses and other critical health workers.”
Meanwhile, legislators are focusing on bolstering certain subspecialties of mental healthcare workers at VA. Legislation passed in October 2020 required VA to create a separate occupational series for licensed professional mental health counselors (LPMHCs) and marriage and family therapists (MFTs) within one year of the law’s passing. Doing this would create separate titles and codes for both professions, ostensibly making it easier for VA to hire these workers and for potential employees to search for these specific jobs.
No Timeline
In a letter sent to VA Secretary Denis McDonough last month, the leaders of the Senate VA Committee noted that VA has yet to provide Congress with a timeline for establishing the two occupational series.
“The absence of an occupational series for these two positions can add difficulties to the hiring process for human resource personnel attempting to fill vacancies and candidates researching and applying for positions at VA,” Senators Jon Tester (D-MT) and Jerry Moran (R-KS) wrote in the letter.
In May, VA reported a 23% vacancy rate among LPMHCs and MFTs. In the OIG report, mental health providers take up two of the top five spots, and social workers are in the top 15.
“This high vacancy rate means VA is less equipped to provide veterans with counseling for PTSD, substance use disorders, military sexual trauma, readjustment to civilian life, marriage and family matters and other issues,” the senators declared.
While VA and the Office of Personnel Management (OPM) said they were establishing a project team to create the occupational series, Congress has not been updated on their progress since November 2021.
“This briefing provided no timeline regarding the [team’s] course of action … and we have received no update on the work,” the senators wrote. “This is also troubling since we have been asking VA and OPM since 2017 to establish an occupational series for these mental health professionals.”
- VA OIG; OIG Determination of Veterans Health Administration’s Occupational Staffing Shortages Fiscal Year 2022, VA OIG Report 22-00722-187, July 7, 2022