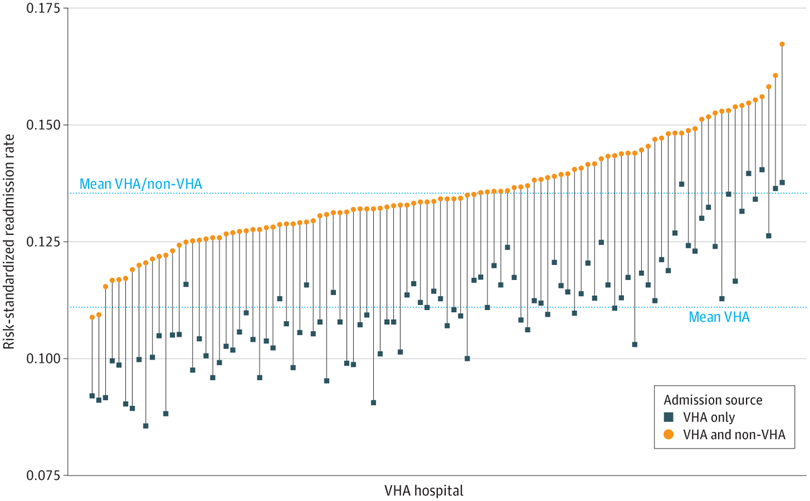
Click to Enlarge: Changes in Hospital Risk-Standardized Readmission Rate Based on Veterans Health Administration (VHA) Readmissions Only vs VHA Plus Non-VHA Readmissions. The change in risk-standardized readmission rate with the addition of non-VHA readmissions is illustrated with vertical lines. The mean VHA-only and the mean VHA plus non-VHA readmission rates are illustrated as horizontal lines. Source JAMA Network Open
IOWA CITY, IA — As the veteran population ages and healthcare options expand, it might be beneficial for the VHA to reassess how it evaluates hospital performance, a new study suggested.
The VHA traditionally assesses its hospitals using metrics such as risk-standardized 30-day readmission rates (RSRR), which track how often patients return for care after surgery. These metrics have historically relied solely on data from VHA hospitals, excluding readmissions that occur in private-sector facilities, however.
With more veterans becoming eligible for Medicare and the expansion of the Care in the Community program—which allows veterans to access non-VA hospitals—a growing number of veterans are seeking care outside the VA system. This shift raises critical questions about how hospital performance is measured.
To determine how readmission to non-VA hospitals might affect RSRR researchers analyzed data from the Veterans Affairs Surgical Quality Improvement Program (VASQIP), encompassing patients aged 65 and older who underwent inpatient surgical procedures at 104 VHA hospitals between 2013 and 2019. To capture comprehensive readmission information, the VASQIP data were linked with patient-level records from both the VHA and Medicare, ensuring inclusion of readmissions to non-VHA hospitals. The study focused on patients who had continuous enrollment in both VHA and Medicare during the year preceding their surgery to maintain data consistency.1
The primary outcome measured was the occurrence of unplanned readmissions to any acute care hospital (VHA or non-VHA) within 30 days following discharge from the index surgical procedure. To evaluate hospital performance, researchers calculated RSRRs for each VA hospital using two models: one considering only VA readmissions and another incorporating both VA and non-VA readmissions. Hospitals were then categorized into quintiles based on their RSRRs from each model, allowing for comparisons and identification of shifts in performance rankings when non-VA readmissions were included.
Out of 108,265 patients included in the study, the overall 30-day readmission rate was 14.0%. Notably, the proportion of readmissions occurring at non-VA hospitals varied significantly across the 104 VHA hospitals, ranging from 0% to 55.3%, with a median of 20.9%, researchers reported in JAMA Network Open.1
When non-VHA readmissions were incorporated into the RSRR calculations, 47.2% of VHA hospitals experienced a change in their performance quintile. Specifically, 24 hospitals (23.1%) improved their ranking by at least one quintile, while 23 hospitals (22.1%) saw a decline by at least one quintile. This indicated that nearly half of the hospitals had their performance assessments altered when accounting for non-VHA readmissions.
Hospitals that improved in performance ranking upon inclusion of non-VHA readmissions tended to have higher surgical volumes and greater complexity in services offered. These hospitals also had a lower proportion of patients receiving care outside the VHA system, suggesting better continuity of care within the VHA network.
“Readmission is a high-priority performance metric that is the focus of national efforts to improve quality of care through public reporting, financial incentives, and oversight,” wrote Mary Vaughan Sarrazin, PhD, an investigator at the Center for Access & Delivery Research and Evaluation (CADRE) at the Iowa City VA, and colleagues.
The increased use of non-VHA services influences VHA hospital performance metrics in two key ways, according to the authors. First, non-VHA services can introduce bias into these measurements. “In our study, hospitals with low non-VHA utilization tended to be unfairly penalized, suggesting that enhancing care continuity might paradoxically lower VHA readmission performance ratings. Conversely, overlooking non-VHA services for certain metrics may penalize hospitals with higher non-VHA utilization (e.g., missing outside cancer screenings).”
“Likewise, comparisons among private-sector health care systems may misrepresent performance if use of external services varies,” the authors continued. “Payer-based assessments, like those reported on CMS Care Compare, encompass all payer-funded services irrespective of location. However, private-sector clinical registries, like the National Surgical Quality Improvement Program, only capture care within a single hospital system. Similarly, VASQIP currently captures care occurring within the VHA.”
The second issue is that VHA hospitals have limited control over the quality of non-VHA services, which can negatively impact performance metrics. The authors noted that poor coordination of post-discharge care, medication changes, or conflicting self-care instructions can elevate the risk of readmission. “Our study found that presurgical care fragmentation was associated with a 10% higher readmission risk, possibly indicating unmeasured risk or adverse effects of fragmented care,” they wrote. “As veterans increasingly access community care, VHA clinicians face greater responsibility for care received outside their facilities. Effective coordination, including information sharing with non-VHA clinicians, is crucial to ensure veterans receive quality care.”
“The VHA’s Office of Integrated Veteran Care, established in October 2021, supports this coordination effort,” the authors added.
The findings highlighted the importance of accounting for out-of-system readmissions when evaluating hospital performance following inpatient surgeries. “Readmission is a high-priority performance metric receiving national attention in quality improvement efforts,” the authors concluded. “As VHA-purchased care continues to increase, the impact of out-of-system readmissions becomes increasingly significant. Our findings have implications for quality assessment within the VHA and external assessments that rely on incomplete data regarding patient services.”
- Vaughan Sarrazin M, Gao Y, Jacobs CA, Jacobs MA, Schmidt S, Davila H, et al. Private-Sector Readmissions for Inpatient Surgery in Veterans Health Administration Hospitals. JAMA Netw Open. 2024 Dec 2;7(12):e2452056. doi: 10.1001/jamanetworkopen.2024.52056. PMID: 39724374; PMCID: PMC11672159.


