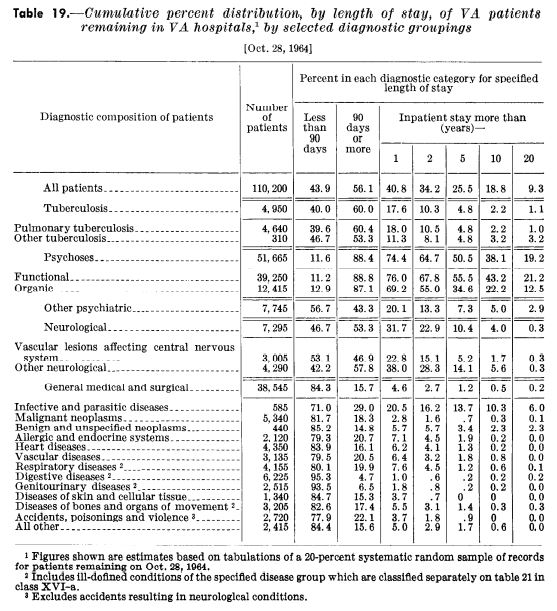
Click to Enlarge: Cumulative percent distribution, by length of stay, of VA patients remaining in VA hospitals, by selected diagnostic groupings Source: Annual
Report ADMINISTRATOR OF VETERANS AFFAIRS, 1965
WASHINGTON, DC — With news every day about VA staffing cuts, the cancellation of contracts and, essentially, the way the agency does business, it is interesting to look back to what might seem to us as a simpler time – 60 years ago, when U.S. Medicine began.
It wasn’t that simple to those living through it, however. Something that would have a dramatic effect on the VA in coming years was that U.S. Marines land on beaches near Da Nang, South Vietnam as the first American combat troops to enter Vietnam and then, a few months later President Lyndon Johnson President called for 50,000 more ground troops to be sent to Vietnam, increasing the draft to 35,000 each month.
Whether administrators knew what was coming or not, VA made significant changes that helped it manage the onslaught of Vietnam veterans in need of care in the future. Interestingly, when W. J. Driver, the VA administrator, submitted the 1965 report to Congress, he touted “a year of change, of adaptation to the current needs of an aging veteran population”
Among the key changes highlighted were:
- the introduction of the nursing care program into VA’s system of medical care;
- the reopening of the National Service Life Insurance program on a limited basis;
- positive steps taken to redesignate and relocate hospital and domiciliary beds to best serve the veteran population; and
- the increasing use of automation in the administration of veterans programs.
An estimated 21,834,000 civilians were potentially eligible on June 30, 1965, for VA benefits and services. A year earlier the estimated number of veterans in civil life had been 21,866,000. The decline possibly represented deaths of more World War I veterans before the onslaught of Vietnam veterans.
The number of veterans reaching age 65 in fiscal year 1965 was 95,000, bringing to more than 2.3 million the total number in this age category.
“All but 12,000 World War I veterans have now attained age 65,” the report noted. “The next 7 or 8 years will provide a lull in the movement of war veterans into the 65 and over age group. Thus, in 1970 the projected older veteran population will be below 2 million. By 1980 however, World War II veterans will swell the total in the 65 and over group to over 3 million.” The actual number was slightly lower, but the prediction was close.
What hasn’t changed, is that veterans were concentrated in certain areas – although those areas have changed over time. As of June 30, 1965, it was estimated that more than half of all veterans in the United States lived in eight States, whereas eleven other States contained only 3 percent of the total U.S. veteran population.
“During the past year analysis was continued on the movement of veterans in order to better plan the future location of VA service facilities,” the study explained. “One result of these studies was the development of projections of the war veteran population of the States in 1970 and 1980. On the basis of assumptions that were made in connection with this analysis, indications (not predictions) were that only two states, Florida and Arizona, will have more war veterans in 1980 than in 1960.”
Florida, with California and Texas, was among the top three states with the most veterans in 2023.
Nursing bed care had been authorized in fiscal year 1964 and expanded by the Congress in fiscal year 1965, became a reality. The result was that about 1,000 nursing beds were placed in operation at 27 VA hospitals and a program was installed for reimbursing state and private nursing homes for providing such care to eligible veterans.
At year end, the VA was operating 168 hospitals with 120,509 beds, 211 outpatient clinics, 18 domiciliaries, 2 restoration centers, and 27 nursing bed care facilities. The 168 VA hospitals contained a total capacity of 120,509 beds. An important new hospital was added during the year — the 710-bed general hospital at Washington, D. C., replacing a 335-bed hospital which had been in operation since 1922.
The agency also recommended the closing of six hospitals and two domiciliaries. An interesting fact, in light of the move toward community care, is that the number of patients treated at the 168 VA hospitals was more than 730,000, but only 24,000 VA patients received care in non-VA hospitals.
Outpatient treatment continued to play a major role in the VA medical program. During fiscal year 1965 outpatients made 4.8 million visits to VA facilities and 1.2 million visits to fee basis physicians.
As new VA Secretary Douglas Collins might attest today, the report advises, “The proper and effective use of people in an agency the size of the Veterans Administration is a never-ending job. New and better ways to perform the mission of the agency are continually looked for and experimented with, keeping always in mind that the goal is service to the veteran. The need for this type of approach can best be understood when one realizes that there were over 167,000 employees in a pay status on June 30, 1965.”
Driver touted the start of an automated personnel and pay system and noted that, by February 1966, VA would have the largest single biweekly automated pay system in the world.
The was just one way automation was beginning to play a key role in healthcare delivery and VA operations.
“Existing systems were expanded and refined, new systems like the one mentioned in the paragraph above were initiated and exploration and analysis of potential areas for possible application continued,” the report detailed. “The first stage of an automated management information system (AMIS) is in operation covering hospital and outpatient clinic data and effective July 1, 1965, the system is being extended to cover other veterans’ benefits programs.”
And the more things change, the more they stay the same. “Effective utilization of manpower continued to be the major task of management personnel in the agency,” Driver reported. “A formal cost reduction program was established to identify areas for cost reduction and to set savings goals.”

