Study Said Housing Is an Important Social Determinant of Health
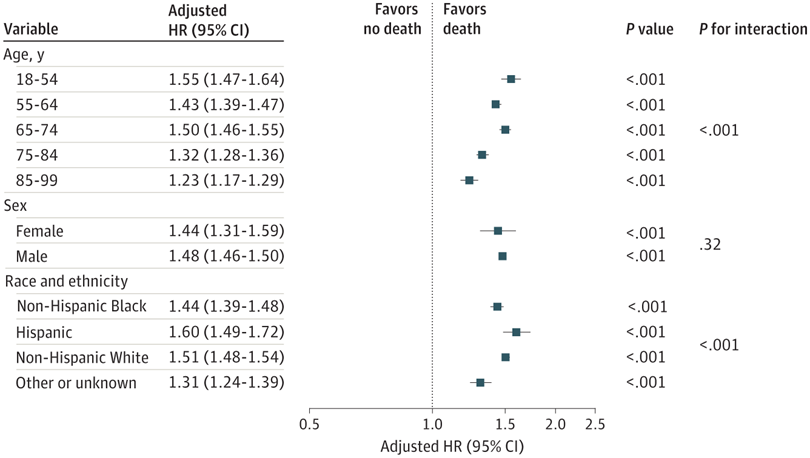
Click to Enlarge: Hazard ratios (HRs) represent the risk of death among veterans experiencing homelessness compared with those not experiencing homelessness. HRs are adjusted for year of incident chronic kidney disease, age, sex, and race and ethnicity and exclude the demographics used as the stratification variables. Error bars denote 95% CIs. Source: JAMA Network Open
ATLANTA — U.S. veterans with a history of homelessness had a much greater risk of end-stage kidney disease (ESKD) and death, according to a new study, underscoring the role of housing as a social determinant of health.
The authors of the cohort study of 836,361 veterans suggested that their findings, reporting in JAMA Network Open, by homeless veterans greater comorbidity burden.1
The study was led by the national Centers for Disease Control and Prevention in Atlanta and included participation from Walter Reed National Military Medical Center, and the Uniformed Services University, both in Bethesda, MD; the VA Healthcare System in Salem, VA, and the VA Salt Lake City Healthcare System, as well as other academic institutions.
“These findings suggest that, among veterans with incident stage 3 to 5 chronic kidney disease, lack of housing may be a major determinant of adverse health outcomes,” the researchers wrote, adding, “Adults experiencing homelessness in the U.S. face numerous challenges, including the management of chronic kidney disease (CKD). The extent of a potentially greater risk of adverse health outcomes in the population with CKD experiencing homelessness has not been adequately explored.”
That led the study team to conduct a retrospective cohort study between Jan. 1, 2005, and Dec. 31, 2017. Participants were veterans with incident stage 3 to 5 CKD who were VHA patients. Patients were followed-up through Dec. 31, 2018, for the occurrence of ESKD and death. Analyses were performed from September 2022 to October 2023.
The patients were determined to be without housing if they had used homeless services at the VA. Defined as primary outcomes were ESKD, based on initiation of kidney replacement therapy, and all-cause death.
Among the 836,361 veterans in the study, the largest proportion was aged 65 to 74 years (274,371 veterans [32.8%]) or 75 to 84 years (270,890 veterans [32.4%]). Nearly all, 96.8%, were male.
Results indicated that 26,037 of the veteran participants (3.1%) developed ESKD, and 359,991 (43.0%) died. Compared with veterans who had not experienced homelessness, those with a history of homelessness showed a significantly greater risk of ESKD (adjusted HR, 1.15; 95% CI, 1.10-1.20), the researchers reported. They also observed a greater risk of all-cause death (HR, 1.48; 95% CI, 1.46-1.50). After further adjusting for body mass index, comorbidities and medication use, the results were attenuated for all-cause death (HR, 1.09; 95% CI, 1.07-1.11) and were no longer significant for ESKD (HR, 1.04; 95% CI, 0.99-1.09), the authors pointed out.
“On any given day in 2023, approximately 653,000 individuals in the U.S .were experiencing homelessness, with 4 in 10 residing in unsheltered locations,” the study advised. “Experiencing homelessness can lead to a variety of adverse health outcomes, including an increased risk of falls, infection, cardiovascular disease, substance use disorder, and death. Chronic kidney disease (CKD) often requires intensive management to limit disease progression and systemic complications through lifestyle modification and/or pharmaceutical treatment. Given the social and economic challenges of homelessness, disease management is expected to be insufficient. Therefore, CKD complications can be of major health consequence among people experiencing homelessness.”
The researchers pointed out that few prior studies have evaluated the risk of end-stage kidney disease (ESKD) or death among populations with CKD experiencing homelessness or with a history of homelessness in the United States. A study last year examined outcomes among veterans with ESKD receiving dialysis and found that unstable housing experienced within 3 years prior to starting dialysis was associated with an increased risk of all-cause mortality.2
Veterans at Greater Risk
The authors suggested that, within the U.S., veterans appear to be at greater risk of homelessness, with 20 per 10,000 veterans experiencing homelessness compared with 18 per 10,000 individuals in the general population.
“In addition, the veteran population may provide practical and unique insight into CKD outcomes among adults experiencing homelessness, given their greater comorbidity burden compared with nonveteran adults experiencing homelessness and veterans’ access to the Veterans Health Administration (VHA), a nationwide health care system from which comprehensive data can be retrieved,” they wrote.
The researchers said they observed a greater risk of both ESKD and death among veterans with a history of homelessness compared with those who did not have a history of homelessness. “Results from secondary analyses suggest that particularly for ESKD, the greater risk may be attributed to a greater comorbidity burden among veterans with a history of homelessness,” they explained. “In analyses exploring time-varying HRs, results were more attenuated in later years of follow-up, particularly for incident ESKD, which did not show significant results after the first 6 years of follow-up. In subgroup analyses evaluating risk of ESKD or death, results differed most substantially by subgroups of age or race and ethnicity for the risk of death.”
The study advised that, although clinical characteristics of the cohort showed substantial differences by homeless status, only some of these factors, such as age and comorbidities, appeared to be greatly associated with risk of ESKD or death. “Adjusting for comorbidities substantially attenuated HRs, suggesting that among all evaluated risk factors, they may contribute the most to risk of ESKD or death,” according to the authors. “These results are consistent with the established role of cardiovascular disease and diabetes as risk factors for progression to ESKD and a high risk of cardiovascular death among adults with CKD. Compared with veterans without a history of homelessness, those with a history of homelessness had a substantially higher prevalence of current smoking and substance use disorder, which may be associated with an increased risk of ESKD or death.”
Because further adjustment for those factors, after accounting for comorbidities, did not substantially affect the results, the researchers said that suggested that other comorbidities might be greater contributors to risk of ESKD and death in the homeless population, adding, “Alternatively, the potential associations of substance use with ESKD and death may have been already accounted for in the regression model after adjustment for other comorbidities.”
The study emphasized that the homeless represent the most socioeconomically disadvantaged population in terms of income, housing, health care access, air pollution exposure, climate change, and other related social determinants of health, adding, “Health outcomes of adults with CKD experiencing homelessness may, therefore, be most affected by homelessness itself, underscoring the role of housing as a fundamental prerequisite for sufficient management of chronic disease.”
Because follow-up care is critical for CKD, the researchers called for future interventions to comprehensively address barriers to healthcare access faced by veterans experiencing homelessness. “These barriers include distrust in health care services, feelings of judgment or stigma from practitioners, prioritizing basic needs such as food and shelter over health care, lack of transportation, and lack of knowledge of available health care resources,” they wrote.
The authors said their study “demonstrated the high risk of adverse health outcomes among veterans with CKD with a history of homelessness, despite comprising a population with access to both health insurance and programs to provide social, financial, and other forms of assistance to individuals experiencing homelessness.” They added that potential interventions to improve CKD management might include tailored outreach to increase access to care in this population, while longer-term solutions will require the recognition of housing as a primary determinant of health and “prioritization of housing to ensure adequate management of CKD and any other chronic conditions.”
- Koyama AK, Nee R, Yu W, et al. Homelessness and Risk of End-Stage Kidney Disease and Death in Veterans With Chronic Kidney Disease. JAMA Netw Open. 2024;7(9):e2431973. doi:10.1001/jamanetworkopen.2024.31973
- Novick TK, Mader MJ, Johansen KL, et al. Unstable housing and mortality among US veterans receiving dialysis. JAMA Netw Open. 2023;6(11):e2344448. doi:10.1001/jamanetworkopen.2023.44448

