Disparities Based on Race, Ethnicity and Other Factors
Click to Enlarge: CAN indicates care assessment need score; CCI, Charlson Comorbidity Index; ESKD, end-stage kidney disease. Source: JAMA Network Open
PALO ALTO, CA — Surgery is a significant healthcare event that necessitates timely planning for goals of care (GOC), involving discussions about one’s current values, aspirations and treatment preferences. Since 2017, the VHA has piloted and coordinated the Life-Sustaining Treatment (LST) Decisions Initiative (LSTDI), aiming to engage healthcare clinicians and patients in conversations and documentation of patients’ desires and preferences regarding various life-prolonging medical treatments and the designation of surrogate decision-makers.
Yet from the national implementation of LSTDI in July 2018 to February 2020, only 3.8% of VHA patients undergoing surgical procedures had completed LST documentation by their surgery date, despite recommendations to initiate the LST process for seriously ill patients at risk of life-threatening events.
A new study published in JAMA Network Open indicated that, while LST documentation rates have increased in a VHA cohort in subsequent years, they remain low overall, with disparities based on a number of factors including race, ethnicity and history of mention health disability.1
To assess the association of race, ethnicity and other factors with disparities in preoperative goals of care documentation among veterans, researchers at the Stanford University School of Medicine and VA Palo Alto Health Care System conducted a retrospective cross-sectional study assessing VHA data from veterans who underwent at least one surgical procedure in the VHA between Jan. 1, 2017, and Oct.r 18, 2022, and were using VHA services for at least one year prior to their surgical procedure.
Using categories created from clinical evaluation of International Statistical Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes and classified by Healthcare Cost and Utilization Project (HCUP) procedure class flags, the researchers included surgical procedures that were defined as major therapeutic or diagnostic procedures performed in the operating room for their analysis. They categorized race into three groups: Black or African American, white and other (including American Indian or Alaskan Native, Asian, Native Hawaiian or Other Pacific Islander) and defined ethnicity as Hispanic vs. non-Hispanic individuals.
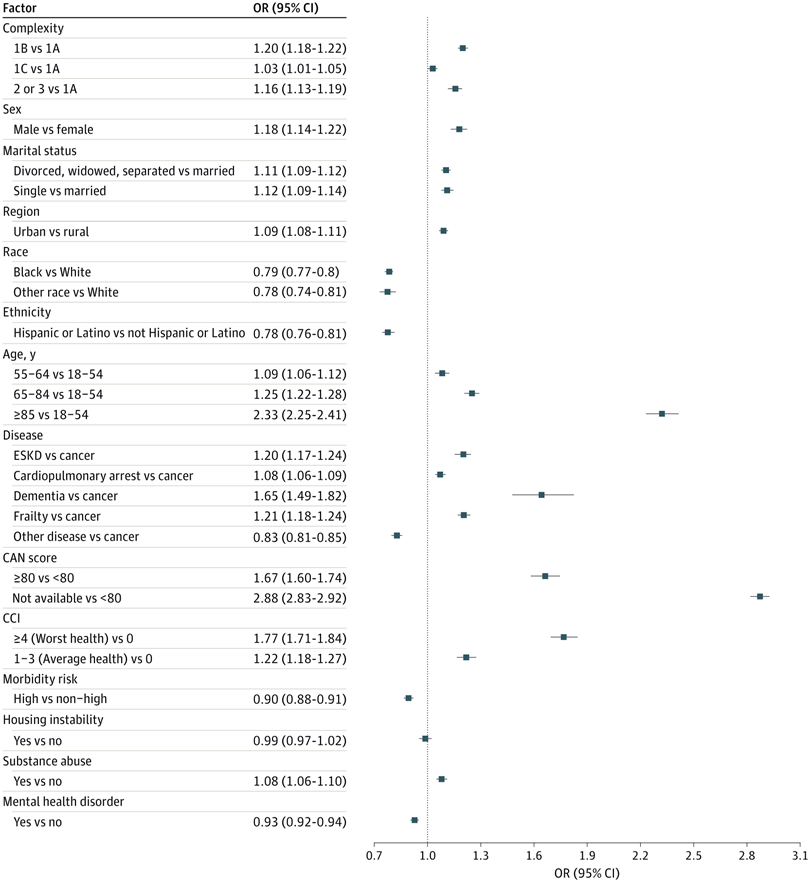
They used logistic regression to analyze the association between the completion of life-sustaining treatment (LST) and various patient characteristics including various patient attributes, such as race, age, gender, marital status, housing stability, rural or urban residency, Care Assessment Need score within one year before the surgery, Charlson Comorbidity Index (CCI) within one year before the surgery, presence of significant medical comorbidities, history of mental health comorbidities and substance-use disorder within the year preceding the surgery.
Differences in Patients With, Without LST Documentation
Of the 229,737 veterans at 130 VA facilities in this study, 13,408 (5.8%) completed an LST note within 30 days before surgery. While standardized mean difference values varied, noteworthy differences were observed in patients with and without documented preoperative LST. In unadjusted analyses, individuals lacking preoperative LST documentation, compared with those with completed documentation, tended to be younger, Black rather than Hispanic, residents of rural areas, with no history of substance use, a history of one or more mental health comorbidities, no history of housing issues and seen at low-complexity, low-volume facilities designated as level 3. Conversely, patients presenting to the highest-complexity facilities designated as level 1A were more likely to complete preoperative LST.
Over the course of the study, unadjusted rates of preoperative LST documentation exhibited a continuous increase: 0.27% in 2017, 4.3% in 2018, 7.0% in 2019, 12.6% in 2020, 16.7% in 2021, and 18.3% in over three quarters of 2022. Notably, patients undergoing surgery after March 11, 2020, the date of the World Health Organization’s declaration of the COVID-19 pandemic, tended to complete preoperative LST documentation more frequently (5484 [40.9%] vs. 28,679 [13.3%]).
“Despite increasing rates of preoperative LST documentation over time, even during the COVID-19 pandemic, a low proportion of patients undergoing surgical procedures overall, particularly individuals from racially and ethnically minoritized communities and patients from rural regions, completed LST documentation before surgery,” the authors wrote. “While there were greater odds of clinicians completing preoperative LST documentation for patients from racially or ethnically minoritized communities at lower-complexity VA facilities, patients undergoing surgical procedures from racially or ethnically minoritized communities, patients with a history of comorbid mental health disorders, and those who live in rural areas were significantly less likely to complete LST documentation.”
Study Offers Opportunities
The authors stated that their study provides several opportunities for healthcare clinicians to engage with individuals from racially and ethnically minoritized communities in GOC discussions and improve preoperative goals documentation.
“Our study reinforces the persistence of racial and ethnic disparities and highlights other patient-level gaps in GOC documentation for the surgical patient population,” they wrote. “Our study also supports the need for future interventions that target patient groups at risk of not engaging in serious illness communication.”
- Wu, A., Giannitrapani, K. F., Garcia, A., Bozkurt, S., et al. (2023). Disparities in Preoperative Goals of Care Documentation in Veterans. JAMA network open, 6(12), e2348235. https://doi.org/10.1001/jamanetworkopen.2023.48235

