VA Disability Compensation Would Be Significantly Affected
Click to Enlarge: Clinical, Occupational, and Financial Outcomes in the United States Calculated with Race-Based versus Race-Neutral Lung-Function Equations.
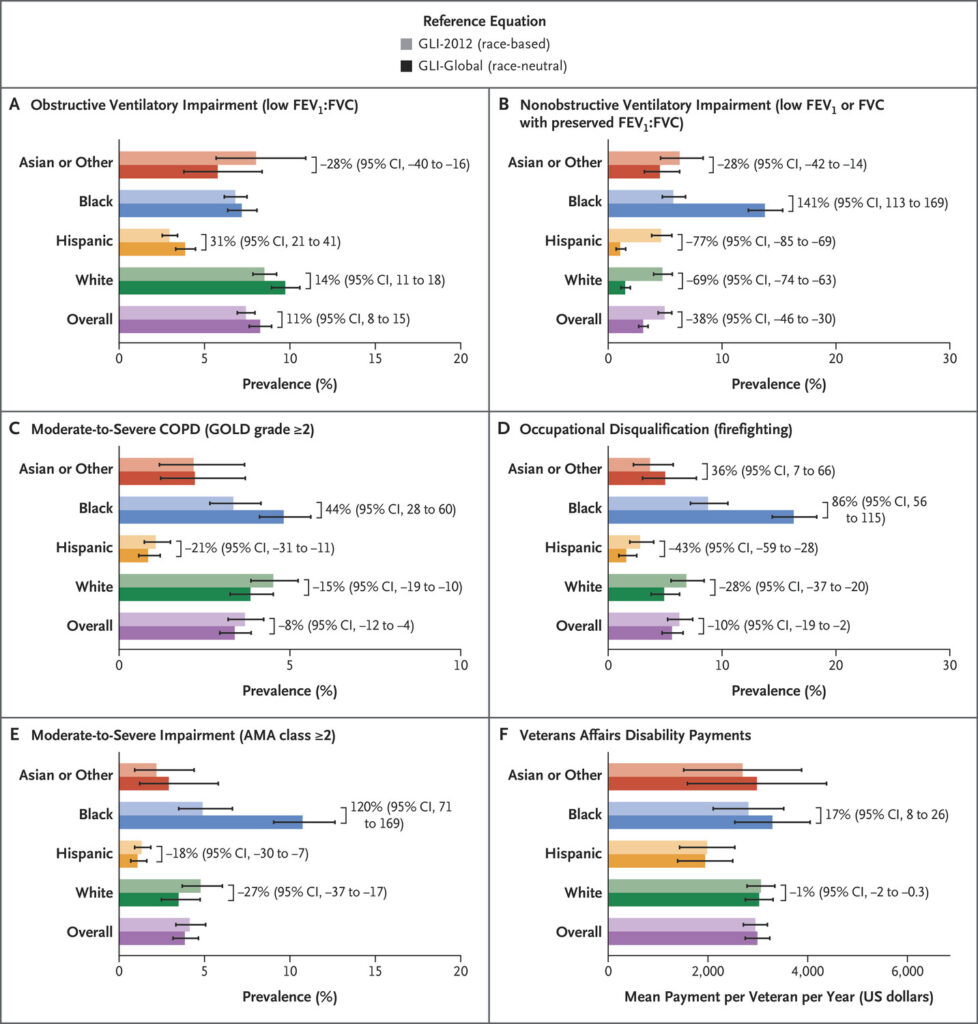
Shown are outcomes for study participants with regard to obstructive ventilatory impairment (Panel A), nonobstructive ventilatory impairment (Panel B), chronic obstructive pulmonary disease (COPD) of grade 2 or higher on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) scale (Panel C), disqualification from firefighting occupations (Panel D), American Medical Association (AMA) impairment classifications (Panel E), and Department of Veterans Affairs disability payments (Panel E) when lung function was interpreted with the use of race-based Global Lung Function Initiative 2012 (GLI-2012) equations and with race-neutral GLI-Global equations. Data from the National Health and Nutrition Examination Survey (NHANES) 2007-2012 were survey-adjusted to be representative of the U.S. population (see the Supplementary Methods section). Error bars represent 95% confidence intervals for outcome values. Numeric labels represent relative changes between the outcomes projected on the basis of GLI-2012 equations (lighter) and GLI-Global equations (darker); confidence intervals overlapping 0 were not labeled. Because outcome values calculated with the use of GLI-2012 and GLI-Global equations are highly correlated, uncertainties in adjacent bars cannot be used to approximate the uncertainty in their difference. Source: New England Journal of Medicine
BOSTON — In 2023, the American Thoracic Society recommended race-neutral interpretation of lung function and requested the investigation of “consequences for the yet-unquantified number of individuals with results near decision-making thresholds.”
A recent study showed that the choice of including or removing adjustment for race does not meaningfully change the discriminative accuracy of relevant clinical outcomes but potentially reclassifies lung diseases, occupational eligibility and disability compensation for millions, according to a new study published in The New England Journal of Medicine.1
Black individuals generally are moved into a more advanced disease category, and white and Hispanic individuals are reclassified as having less advanced illness, according to the study. VA disability payments could be especially impacted, according to the study.
The Global Lung Function Initiative (GLI), which brings together physiologists, respiratory experts, epidemiologists and statisticians, is pushing to change how lung function tests are interpreted. In 2022, GLI replaced race-based equations with race-neutral ones. The updated equations also have been endorsed by the American Thoracic Society and the European Respiratory Society.
For the study looking at the effects of that shift, Harvard University-led researchers obtained longitudinal data from 369,077 participants in the National Health and Nutrition Examination Survey, U.K. Biobank, the Multi-Ethnic Study of Atherosclerosis and the Organ Procurement and Transplantation Network and used them to compare the race-based 2012 Global Lung Function Initiative (GLI-2012) equations with race-neutral equations introduced in 2022 (GLI-Global).
The results indicated that, among the 249 million individuals in the United States between 6 and 79 years of age who are able to produce high-quality spirometric results, the use of GLI-Global equations could reclassify ventilatory impairment for 12.5 million persons, medical impairment ratings for 8.16 million, occupational eligibility for 2.28 million, grading of chronic obstructive pulmonary disease for 2.05 million and military disability compensation for 413,000.
“These potential changes differed according to race; for example, classifications of nonobstructive ventilatory impairment may change dramatically, increasing 141% (95% confidence interval [CI], 113 to 169) among Black persons and decreasing 69% (95% CI, 63 to 74) among white persons,” the authors pointed out. “Annual disability payments may increase by more than $1 billion among Black veterans and decrease by $0.5 billion among white veterans.”
They added that GLI-2012 and GLI-Global equations had similar discriminative accuracy with respiratory symptoms, healthcare utilization, new-onset disease, death from any cause, death related to respiratory disease and death among persons on a transplant waiting list, with differences in C statistics ranging from −0.008 to 0.011.
“The use of race-based and race-neutral equations generated similarly accurate predictions of respiratory outcomes but assigned different disease classifications, occupational eligibility, and disability compensation for millions of persons, with effects diverging according to race,” according to the researchers.
Specifically, the report described how VA disability payments are determined in part on the basis of spirometric criteria and what effect that would have. “The use of GLI-Global equations to calculate compensation for respiratory impairment associated with military service among Black veterans may increase payments by 17.1% (95% CI, 8.5 to 25.8) amounting to $1.10 billion (95% CI, 0.58 billion to 1.61 billion) annually,” according to the report. “Among the 216,000 Black veterans (9.5%) who stand to benefit, annual compensation could increase by $1,991 for 37.0% of that population, by $4,110 for 41.1%, by $9,740 for 19.0%, and by $27,600 for 2.9%.”
On the other hand, the study pointed out, compensation could decrease by 1.15% (95% CI, 0.29 to 2.00) among white veterans, amounting to $0.52 billion (95% CI, 0.13 billion to 0.92 billion. For the 150,000 white veterans (1.0%) who would be affected, annual compensation would decrease by $1,991 for 28.8% and $4,110 for the remaining 71.2%.
Redistributing VA Disability Benefits
“In total, the use of GLI-Global equations may redistribute $1.94 billion (95% CI, 1.10 billion to 2.79 billion) in annual VA disability compensation among 413,000 veteran recipients,” the authors wrote. “The redistributed amount is less than 2% of the total VA disability compensation spending reported in 2022 but probably represents a sizable proportion of the spending on respiratory conditions, which accounts for less than 5% of all service-connected disabilities among veterans.”
Expected spirometry values tend to differ by race, with lower scores expected for Black individuals, but current interpretation of spirometry test results has relied only on reference ranges that reflect assumptions of innate differences in lung function among races, according to a Harvard Medical School press release on the study.
“The race-based formula to estimate lung function assumes that different race groups have different normal lung function, and it’s known that this can obscure disease severity in many individuals,” Raj Manrai, PhD, the study senior author and assistant professor of biomedical informatics in the Blavatnik Institute at Harvard Medical School, said in the press release. “Yet the myriad implications of race adjustment and the effects of removing race have not been comprehensively quantified – our study is an attempt do so.”
“Removing race from current lung function estimates would change who is diagnosed with respiratory illness and, in turn, who qualifies for disability compensation and veterans’ benefits and who’s eligible for jobs that require certain levels of lung function. The researchers suggest that adjusting lung function tests to include race—as has been the case historically—likely normalized worse lung function and downplayed disease severity among Black people,” the study authors explained in the press release.
“These findings underscore the extent of medical decision-making that is at stake with the use of race-based equations and warrant thoughtful consideration of the trade-offs involved,” the authors explained.
Based on the race category that a person was assigned in the GLI taxonomy, the “impact of including or removing adjustment for race or ethnic group for patients is expected to vary. When race-neutral equations were used instead of race-based equations, Black participants in the study were classified as having greater ventilatory and medical impairment, more-severe COPD grades, more frequent occupational disqualifications, and higher amounts of disability payments. Meanwhile, Hispanic and white participants were classified as having opposing changes,” the authors pointed out.
The study found that the “only exception was an increased prevalence of obstructive impairment among Hispanic and White participants, which was the result of obstruction being determined on the basis of the forced expiratory volume in 1 second (FEV1): forced vital capacity (FVC) lower limit of the normal range, which increased for most race groups.”
Overall, the study showed the “use of race in lung-function testing has broad clinical, occupational and financial implications for millions of patients. Further study is needed to explain whether new impairment findings represent false positives or true undetected disease. Additional research is also needed to clarify findings of decreased impairment among healthy Hispanic and white individuals. The authors hope that data on the nature and extent of these implications may inform improvements to current reference equations and preparations for expected changes to care.”
These findings are “relevant to clinicians who treat patients with lung disease, pulmonary function laboratories and hospital administrators, who will need to plan for changes in patient volume stemming from disease severity reclassifications,” according to the Harvard Medical School press release.
- Diao JA, He Y, Khazanchi R, Nguemeni Tiako et. Al . Implications of Race Adjustment in Lung-Function Equations. N Engl J Med. 2024 Jun 13;390(22):2083-2097. doi: 10.1056/NEJMsa2311809. Epub 2024 May 19. PMID: 38767252; PMCID: PMC11305821.
