
In 2012, clinicians with the Forward Surgical Team assigned to Forward Operating Base Wright performed surgery on a trauma patient at the installation’s medical center in Afghanistan. A new study looked at the change in the use of non-therapeutic laparotomy in severely injured military personnel. Photo by the 94th Airlift Wing
BETHESDA, MD — As combat casualty care improved over time during the wars in Iraq and Afghanistan, the use of nontherapeutic laparotomy (NTL) decreased. But exploratory laparotomies remain an important tool in settings where modern imaging modalities are unavailable, according to a new study.
Prior studies of combat casualties reported nontherapeutic laparotomy (NTL) rates as high as 32%, occurring when there is a suspicion of intra-abdominal injury, according to the report in Surgical Endoscopy.1
Researchers from Walter Reed National Military Medical Center, the Uniformed Services University of the Health Sciences and the Henry M. Jackson Foundation for the Advancement of Military Medicine Inc., all in Bethesda, MD, the Brooke Army Medical Center, JBSA, in Fort Sam Houston, TX, and Texas Health Resources in Fort Worth, TX, assessed military personnel with combat-related injuries (6/1/2009-12/31/2014) who underwent exploratory laparotomy based on concern for abdominal injury. All were evacuated to Landstuhl Regional Medical Center in Germany before being transferred to participating U.S. military hospitals.
An NTL was defined as a negative laparotomy without substantial intra-abdominal injuries requiring repair and not performed for proximal vascular control or fecal diversion. The study team examined characteristics, indications for laparotomy, operative findings and outcomes of the procedures.
Their results indicated that, among 244 patients who underwent laparotomies, 41 (16.8%) had NTLs and 203 (83.2%) had therapeutic laparotomies (i.e., positive findings). Patients with NTLs had more computed tomography scans because of concerns about injury (48.8% vs. 27.1%; p = 0.006), less penetrating injury mechanisms (43.9% vs. 71.9%; p < 0.001) and lower Injury Severity Scores (26 vs. 33; p = 0.003) compared to patients with therapeutic laparotomies.
In addition, patients with NTLs were also less likely to be admitted to the intensive care unit (70.7 vs. 89.2% for patients with therapeutic laparotomies; p = 0.007). “No patients with NTLs developed abdominal surgical site infections (SSI) compared to 16.7% of patients with therapeutic laparotomies (p = 0.002),” the researchers advised, adding, “There was no significant difference in mortality between the groups (p = 0.198).”
The study concluded that the proportion of NTLs “was lower than reported from earlier years during the wars in Iraq and Afghanistan. No infectious complications from NTLs (i.e., abdominal SSIs) were identified. Nevertheless, surgeons should continue to have a low threshold for exploratory laparotomy in military patients in austere settings with concern for intra-abdominal injury.”
Background information in the article explained that, in combat settings, penetrating trauma from explosive blasts and high-velocity gunshot wounds can often result in severe intra-abdominal injuries. “Rapid diagnosis and management of abdominal trauma are crucial as delays can result in significant morbidity and mortality,” the authors pointed out. “Modern imaging modalities, such as computed tomography (CT) scans, are frequently unavailable in austere combat environments. Adjuncts, such as ultrasound or diagnostic peritoneal aspiration, can be helpful, but may result in equivocal findings. As a result, surgeons must often rely solely on physical examination and their judgment when deciding whether to perform an exploratory laparotomy. While this approach can be lifesaving, it also risks conducting non-therapeutic surgeries, which may result in the development of complications, such as surgical site infections (SSI), during a patient’s course of care.”
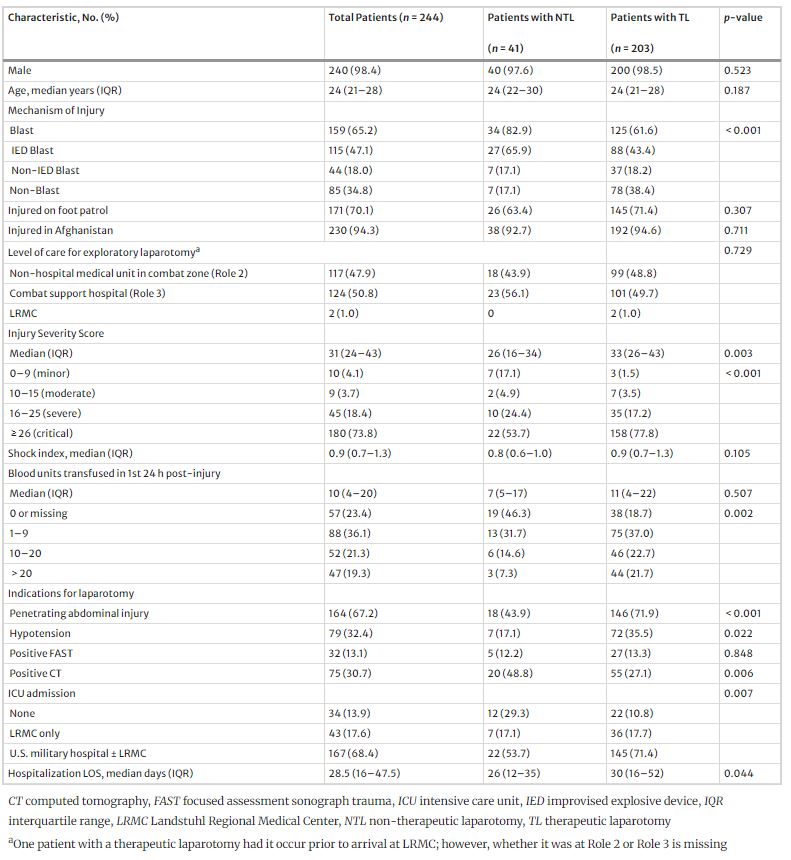
Click to Enlarge: Characteristics of combat casualties who underwent exploratory laparotomies with diagnostic uncertainty Source: Springer Link: Surgical Endoscopy
That was especially the case early in the Iraq and Afghanistan wars because of the high frequency of blast trauma. After nearly a decade of combat, the occurrence of nontherapeutic laparotomies (NTLs) was assessed among U.S. and U.K. combat casualties, and, from 2002 to 2011, 32% of 1,273 laparotomies performed among wounded U.S. military personnel were found to be NTL. A higher proportion occurred among casualties wounded in Afghanistan (38.2% vs. 28.6% in Iraq) and peaked from 2007 to 2010.
Among 130 wounded U.K. military personnel (2003-2011) who underwent a laparotomy, 20.8% were NTLs.
Advances in Combat Care
“While the number of overall laparotomies increased over the study years, the proportion of NTLs showed a downward trend,” the researchers wrote. “Given the early trends of NTLs, advances in combat casualty care and increased availability of resources (i.e. CT scan) as the military trauma system matured, we sought to examine the occurrence and characteristics of NTLs from the later years of the conflicts in Iraq and Afghanistan (2009–2014). The results could help inform guidelines and areas for performance improvements with combat casualty care.”
The authors said their findings offer important perspectives on the frequency and outcomes of NTLs in combat casualties during the later years of the wars in Iraq and Afghanistan, explaining, “The 16.8% proportion of NTLs identified in our population is notably lower compared to previously reported data.” Some past studies suggested that as much as 35% of combat casualties who had laparotomies conducted for indications other than proximal control (2009-2011) had negative findings.
That the current research demonstrates a lower proportion of NTLs “is indicative of the iterative advancements in combat casualty care, growing experience of the deployed surgeons, countermeasures to include improved body armor, and maturation of the military trauma system with increases in available resources. Furthermore, it mirrors the evolution and refinement of Joint Trauma System clinical practice guidelines as more evidence becomes available.”
The report advised that military trauma research generally exhibits higher rates of NTLs compared to civilian trauma settings. For example a study of patients in an urban Level 1 trauma center from 1998-2001 found that only 6% underwent NTLs, and another study found that only 3.9% of 1,871 laparotomies conducted in their study group between 2003 and 2008 were identified as NTL.
“The occurrence of NTLs at civilian centers may be affected by use of routine laparotomies related to injury mechanisms (e.g., generally higher rate of NTLs with abdominal stab wounds versus abdominal gunshot wounds),” the authors stated. “Overall, our finding of a 16.8% proportion of NTLs aligns with expectations within the military context as being elevated in comparison to civilian data, which is not unexpected, given the austere, resource-limited settings in which surgeons often operate. Complicating the military environment is the gap in surgical care during evacuation of the casualty to the next level of care.”
The current study also identified differences in specific pre-operative clinical and radiographic indicators between the patients who had an NTL versus a therapeutic laparotomy. “In particular, “ the authors explained, “nearly 50% of patients with NTLs had a false-positive CT scan indicative of a transperitoneal trajectory with no injuries requiring intervention identified upon exploration, in contrast to 27% among patients with therapeutic laparotomies. This calls into question whether metallic fragmentation from the higher proportion of IED blasts among the patients with NTLs (66% vs. 43%) might compromise the precise determination of peritoneal violation via CT scanning.”
The article also discussed continuing questions about the efficacy of CT scans in military abdominal trauma. It noted that a recent meta-analysis “found that CT scans provided excellent diagnostic accuracy with military abdominal trauma; however, the authors noted the limited number of studies available for inclusion in the meta-analysis and that the types of abdominal injuries were not always well-described in the studies. Selective use of nonoperative management is restricted in military scenarios due to extended transport times and scarce resources for monitoring, as well as the potential lethal consequences for missed intra-abdominal injuries. Thus, further analysis of CT results with greater detail is warranted to identify the limitations of CT scans and develop best practices for their use in combat settings, particularly given advancements in CT technology.”
The researchers also highlighted the absence of surgical-site infections (SSIs) in the NTL group, suggest that was interesting “given the cases were likely not the most sterile procedures. Analysis of combat-related laparotomies conducted for indications other than proximal control reported 4% with wound infections and 3% with intra-abdominal abscesses; however, only 35% of the laparotomies were classified as nontherapeutic. However, similar to our findings, a prior examination of U.S. military personnel with NTLs reported one intra-abdominal abscess and zero wound infections.”
They pointed out that no patients with an NTL in their study were left with a post-operative open abdomen, “which may have contributed to the lack of SSIs. Moreover, while a high proportion (71%) of patients in the NTL group were admitted to the ICU in our study, the need for ICU support was less than what was required for patients with therapeutic laparotomies.”
As for the future of the use of NTLs, the study team predicted they would persist in combat settings. “The clinical presentation of combat patients requiring exploratory laparotomy for abdominal trauma can be obfuscated by multiple factors, such as concurrent injuries, the urgent need for decision-making, and potentially ambiguous pre-operative evaluations. Advancing our understanding through further research is important to refine triage criteria and pinpoint low-risk patients suitable for observation over surgery. Yet, it must be emphasized that in uncertain cases, exploratory laparotomy remains an indispensable intervention in optimizing survival in deployed environments.”
- Walker, P.F., Bozzay, J.D., Schechtman, D.W. et al. Non-therapeutic laparotomies in military trauma (2009–2014). Surg Endosc (2024). https://doi.org/10.1007/s00464-024-11102-4

