WASHINGTON, DC — VA is slowly catching up on the appointments that were canceled in 2020 and 2021 due to the COVID-19 pandemic shutting down many nonessential services at VA hospitals. According to a recent VA Office of the Inspector General (OIG) report, however, glitches remain in the VA system that can allow some veterans’ cases to fall through the cracks.
Between March 2020 and August 2021, about 5.15 million VA patients had more than 35 million appointments canceled. In 2020, the OIG reported that VA had not followed up on nearly one-third of them.
In response, VA implemented the Canceled Appointments and Consult Management Initiative (CACMI) to monitor follow-up for canceled appointments. As the number of veterans who had received follow-up increased, VA transitioned to a post-CACMI sustainment model. This includes a data-monitoring tool that generates a report allowing VA medical facilities to track 11 types of follow-up activities for appointments that were canceled by the facility, canceled by patients with COVID-19 and no-shows.
Those activities, any of which can cause the VA to consider the case closed, include rescheduling the appointment, conversion to telehealth or video appointments and correspondence sent to patients, reminding them to schedule appointments, among others.
OIG investigators questioned, however, whether this tool gives an accurate picture of patient follow-up.
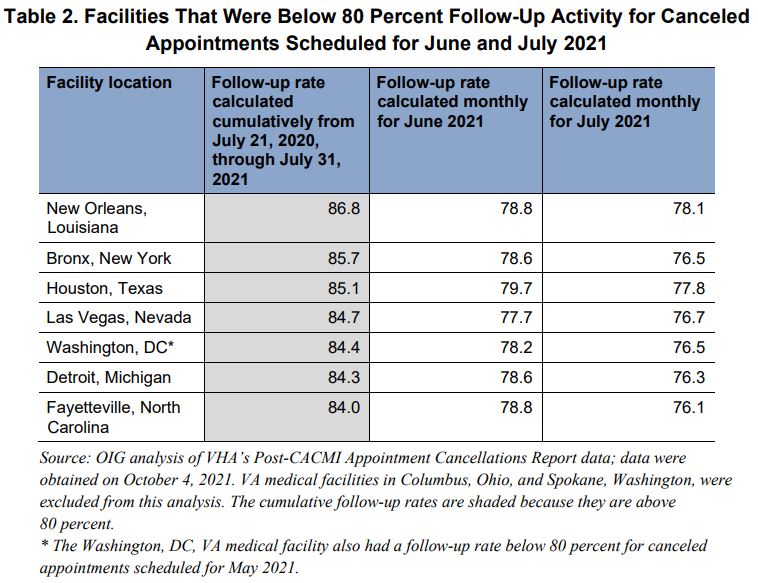
The VA watchdog group evaluated canceled appointments scheduled to occur from Jan. 1 through July 31, 2021. Of those, 8.7 million canceled appointments, VA had evidence of follow-up on 87% of them. According to VA policy, if evidence of follow-up for canceled appointments at a facility ever falls below 80% for two consecutive months, that facility is expected to create an action plan to address the problem.
Investigators found that, while the big picture showed a marked improvement in VA’s follow-up of veterans from 2020, a closer look at the numbers and at the post-CACMI reporting model itself found gaps in the system.
Examining the follow-up activities noted in the patient record, OIG found that 77% of the time the activity was “appointment rescheduled,” which is the primary goal. Other activities included “Return to Clinic,” “Has Visit” and “No Action Other Reason,” the latter being particularly concerning to OIG.
“The team evaluated the patient records for two canceled appointments with ‘No Action Other Reason’ as the evidence of follow-up and determined in both cases medical facility staff did not follow policy to reschedule,” the investigators stated in the report. “In one case, the patient record had evidence that a facility staff member rescheduled the appointment, without the veteran’s input, and left a voice message, which violated VHA policy against blind scheduling. The other case also violated policy because there was no evidence in the patient’s record of further efforts to reschedule an appointment after a patient did not attend the initial appointment.”
The question whether these activity codes are a good way of tracking follow-up remains unanswered. OIG found that, since the post-CACMI data report’s inception, none of the activities have ever been evaluated for effectiveness.
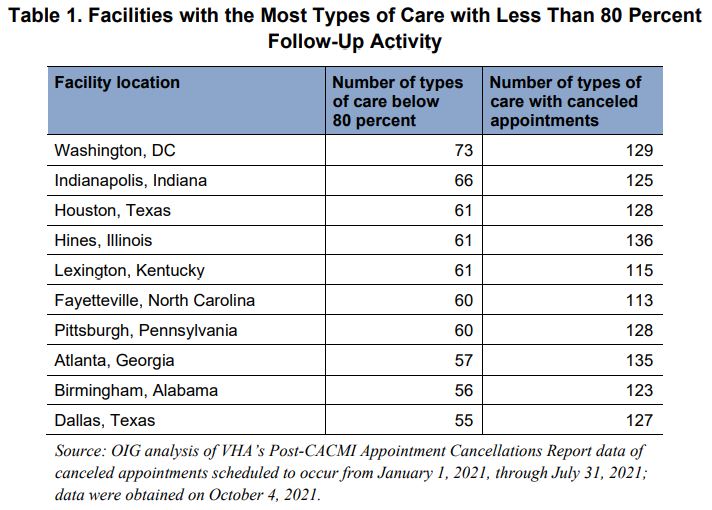
The investigators also found that some types of appointments had poorer follow-up than others. Of the 243 types of care the team looked at, 92 of them had less than an 80% follow-up rate. Those included: mammography (64%), ultrasound (68.5%), women’s preventive care (70.4%), computed tomography scan (73.2%) and nuclear medicine and positron emission tomography (75.4%). According to the report, OIG found that every VA facility reviewed had at least one type of care with a follow-up rate below 80%.
OIG recommended that, if VA continues using this method of follow-up tracking, it should evaluate all the metrics used. And, since they are already gathering the data, the department should drill down into follow-up on specific types of care to get a better understanding of how facilities are actually doing.