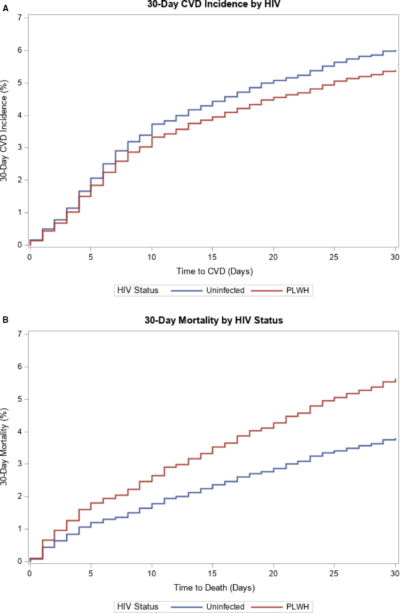
Adjusted* cumulative incidence plots for CVD events and mortality; from hospitalization through 30 days post‐discharge.
A, Cumulative incidence plot showing similar adjusted CVD incidence in PLWH compared with uninfected patients following CAP hospitalization (P=0.33).* adjusted for age, severe CAP, race/ethnicity, prior CAP, diabetes mellitus, hypertension, dyslipidemia, smoking status, alcohol abuse, and illicit drug use. B, Cumulative incidence plot showing higher adjusted 30‐day mortality in PLWH compared with uninfected patients following CAP hospitalization (P=0.002). CAP indicates community‐acquired pneumonia; CVD, cardiovascular disease; and PLWH, people living with HIV.
PHILADELPHIA — HIV patients on anti-retroviral therapy are at increased risk for cardiovascular events, heightening the importance of preventive care. Now, new research has found that selection of blood pressure medication is critically important for this group and can have a significant effect on risk of cardiovascular events or even death.
A VA study found that the type of medication initiated for veterans with HIV appeared to influence risk of heart disease, stroke and heart failure, according to a report in Hypertension, an American Heart Association journal.1
The issue is especially important because patients receiving anti-retroviral therapy (ART) are more likely to develop hypertension and related cardiac issues than those who do not have HIV, according to authors from the Corporal Michael J. Crescenz VAMC and the Perelman School of Medicine at the University of Pennsylvania, both in Philadelphia, and colleagues.
Researchers touted their study as the first to examine how the choice of blood pressure medications influences the long-term risk of heart disease, stroke and heart failure in the HIV positive population with a higher risk of cardiovascular disease.
“We suspected there could be differences in risk based on which medications providers select to treat hypertension among people with HIV due to potential interactions between blood pressure medications and some therapies used to treat the virus,” explained lead author Jordana B. Cohen, MD. “Additionally, factors such as how the body handles salt, inflammation and the accelerated aging of blood vessels may affect the risk of cardiac events in people with HIV differently than people who do not have HIV, which could be influenced by which blood pressure medication is used.”
Among veterans with HIV and incident hypertension using 2000-2018 records, the study team evaluated risk of: (1) incident/recurrent CVD or death, (2) incident CVD and (3) incident heart failure by antihypertensive class. Among 8,041 patients:
- 24% were initiated on ACE (angiotensin-converting enzyme) inhibitor/ARB (angiotensin receptor blocker) monotherapy,
- 23% on thiazide/thiazide-like diuretic monotherapy,
- 13% on β-blocker monotherapy, and
- 11% on calcium channel blocker monotherapy.
Researchers reported that, over a median of 6.5 years, 25% veterans with HIV experienced a CVD event, adding, “β-blockers, but not calcium channel blockers or diuretics, were associated with an increased risk of incident CVD compared with ACEs/ARBs (hazard ratio [95% CI], β-blockers 1.90 [1.24-2.89]; calcium channel blockers 1.02 [0.77-1.34]; diuretics 1.06 [0.86-1.31]); similar hazard ratio were noted for incident/recurrent CVD or death.”
Study participants had an average age 53 years, were 97% male, and 49% were Black.
The report added that, in veterans without chronic kidney disease, ACE inhibitor/ARBs were associated with a lower risk of incident heart failure compared with all other classes (hazard ratio [95% CI]: β-blockers, 1.52 [1.11–2.09]; calcium channel blockers 1.48 [1.00–2.19]; diuretics 1.52 [1.07–2.16]).
“In conclusion, we observed high rates of CVD events in people with HIV with hypertension and a high prevalence of β-blocker use for initial hypertension management, even among those without indications,” the authors wrote. “Our findings highlight the potential harm associated with β-blockers and the possible benefit associated with ACE inhibitor/ARBs for hypertension management in people with HIV. Prospective and randomized trials are needed to confirm these findings.”
“Blood pressure and heart disease risk in patients who have HIV can be safely managed with first-line treatment of hypertension with ACEis, ARBs, CCBs and thiazide diuretics and may have added benefit from initial treatment with ACEis and ARBs,” Cohen added.
The authors pointed out an unusual trend in the group: Although CCBs are among the medications recommended for the initial treatment of hypertension, beta-blockers were prescribed more frequently than CCBs in this VA study.
“We were surprised by the high rates of beta-blockers prescribed for first-line hypertension treatment, since they are not recommended as first-line agents,” Cohen said. “We suspect this may be due to the fact that many people with HIV receive primary care from their infectious disease team, who do an amazing job at managing HIV but may not be focused on blood pressure treatment guidelines and contraindications. Ideally, a patient’s primary care and infectious disease team should work together for the best possible outcomes.”
She raised concerns of possible harm from using beta-blockers as first-line treatment for hypertension despite HIV status.
“Patients with HIV need heightened attention to their elevated risk of heart disease. More dedicated research studying the unique needs for people with HIV and those taking ARTs is needed in order to optimize cardiovascular prevention,” Cohen said.
Pneumonia Risks With HIV
Other recent VA research pointed out how, because of increased CVD risk, community acquired pneumonia is especially risky for veterans with HIV. The research led by Tulane University School of Medicine in New Orleans and including participation from VAMCs in West Haven, CT; Houston; Atlanta; Dallas; Los Angeles; Pittsburgh; Bronx, NY; Nashville, TN; and Seattle, WA, found substantially higher mortality risks for HIV-positive veterans with CAP.
“Hospitalization with community-acquired pneumonia (CAP) is associated with an increased risk of cardiovascular disease (CVD) events in patients uninfected with HIV,” wrote the authors, who sought to determine whether HIV increased the risk of CVD or mortality compared to those without HIV. Their results were published in the Journal of the American Heart Association.2
Data from the Veterans Aging Cohort Study on 4,384 patients admitted with their first episode of CAP from April 2003 through December 2014 was included. Most of those veterans, 67%, were positive for HIV. The patients with HIV were younger, had less severe CAP and had fewer CVD risk factors than patients with CAP who were uninfected with HIV.
Results indicated that, while CVD risk was similar in veterans with HIV compared with the HIV-uninfected (hazard ratio [HR], 0.89; 95% CI, 0.70-1.12), HIV infection was associated with higher mortality risk (HR, 1.49; 95% CI, 1.16-1.90). In models stratified by HIV status.
In addition, researchers reported that CAP severity was significantly associated with incident CVD and 30-day mortality in both the HIV patients and those uninfected.
“Conclusions In this study, the risk of CVD events during or after hospitalization for CAP was similar in [people living with HIV] and patients uninfected with HIV, after adjusting for known CVD risk factors and CAP severity,” the authors wrote. “HIV infection, however, was associated with increased 30-day mortality after CAP hospitalization in multivariable-adjusted models. PLWH should be included in future studies evaluating mechanisms and prevention of CVD events after CAP.”
- Rethy LB, Feinstein MJ, Achenbach CJ, Townsend RR, Bress AP, Shah SJ, Cohen JB. Antihypertensive Class and Cardiovascular Outcomes in Patients With HIV and Hypertension. Hypertension. 2021 Apr 5:HYPERTENSIONAHA12016263. doi: 10.1161/HYPERTENSIONAHA.120.16263. Epub ahead of print. PMID: 33813847.
- Zifodya JS, Duncan MS, So-Armah KA, Attia EF, et. Al. Community-Acquired Pneumonia and Risk of Cardiovascular Events in People Living With HIV. J Am Heart Assoc. 2020 Dec;9(23):e017645. doi: 10.1161/JAHA.120.017645. Epub 2020 Nov 23. PMID: 33222591; PMCID: PMC7763776.


