Adherence to Oral Medications Often a Problem for Veterans
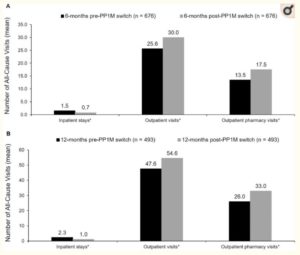
Comparison of all-cause health care resource utilization during the 6 months (A) and 12 months (B) pre- and post-once-monthly paliperidone palmitate (PP1M) switch among patients who initiated treatment with oral risperidone or paliperidone. *P < 0.05.
SEATTLE — Schizophrenia can be frightening and life-changing. Common symptoms such as disorganized thinking and speech, lack of expressive emotion, social withdrawal, neglect of self-care, hallucinations and delusions alienate individuals with schizophrenia from others and create barriers to day-to-day functioning in society.
Compounding the problem is that oral antipsychotics alleviate symptoms in up to 80% of patients, but about half of patients who respond to treatment are nonadherent.
Nonadherence is a major issue with the VA, as an estimated 11% of veterans in VA care suffer from schizophrenia. Nonadherence drives up costs by increasing the need for emergency care and leads to poorer quality of care. When patients don’t follow their drug regimens, providers might mistakenly believe they need different dosages or type of medication or that they are treatment resistant. That results in tremendous human cost in terms of lost jobs, homelessness, social isolation and worse.
“The rates of medication nonadherence is very high and the consequences are very serious for patients with severe mental illness,” Andrew J. Saxon, MD, director of the Center of Excellence in Substance Addiction Treatment and Education, VA Puget Sound Health Care System, told U.S. Medicine.
Saxon, who is also a professor in the department of psychiatry and behavioral health at the University of Washington School of Medicine in Seattle, added, “A patient who relapses could end up in the hospital and they are at higher risk for suicide.”
A recent study of veterans with schizophrenia who switched from daily oral antipsychotics to long-acting injectable (LAI) therapies found that once-monthly injections improve adherence and reduce costs.1
The researchers evaluated records from the VHA database of veterans with a diagnosis of schizophrenia who were initially treated with oral risperidone or paliperidone and switched directly to once-monthly paliperidone palmitate injections.
The study divided veterans into two cohorts. The first cohort of 676 patients began treatment with one of the oral antipsychotics between July 1, 2014, and Sept. 30, 2017, and had continuous care for at least six months before and after the date of medication change. The second cohort of 493 veterans initiated treatment with oral risperidone or paliperidone between Jan. 1, 2015, and March 31, 2017, and had continuous healthcare for 12 months before and after the date of medication switch.
Continue Reading this Article: Adherence Improved

