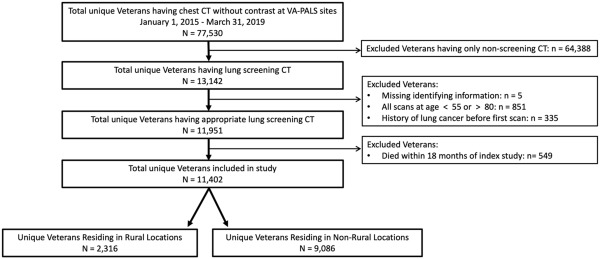
Click To Enlarge: Study cohort. VA-PALS = Veterans Affairs Partnership to Increase Access to Lung Screening. Source: Spalluto LB, Lewis JA, Samuels LR, Callaway-Lane C, et. al. Association of Rurality With Annual Repeat Lung Cancer Screening in the Veterans Health Administration. J Am Coll Radiol. 2022 Jan;19(1 Pt B):131-138. doi: 10.1016/j.jacr.2021.08.027. PMID: 35033300.
NASHVILLE, TN — Repeat lung cancer screening lags among rural veterans and could help explain known disparities in outcomes, according to a new study.
The report in the Journal of the American College of Radiology points out that lung cancer causes the largest number of cancer-related deaths in the United States and that incidence rates, mortality rates and rates of advanced stage disease are all higher among residents of rural areas.1
“Known disparities in lung cancer outcomes between rural and nonrural populations may be in part because of barriers faced by rural populations,” according to authors from the VA Tennessee Valley Health Care System in Nashville and colleagues. The study team tested the hypothesis that, among veterans who receive initial lung cancer screening, rural residents would be less likely to complete annual repeat screening than nonrural residents.
To determine that, researchers conducted a retrospective cohort study of 10 VAMCs from 2015 to 2019, identifying rural and nonrural veterans who underwent lung cancer screening. Rural status was determined using the rural-urban commuting area codes.
Defined as the primary outcome was annual repeat lung cancer screening in the 9- to 15-month window (primary analysis) and 31-day to 18-month window (sensitivity analysis) after the first documented lung cancer screening.
In the final analytic sample of 11,402 veterans, results indicate that annual repeat lung cancer screening occurred in 27.7% of rural veterans (641 of 2,316) and 31.8% of nonrural veterans (2,891 of 9,086) (adjusted odds ratio: 0.86; 95% confidence interval: 0.73-1.03).
The researchers reported that similar results were documented in the sensitivity analysis, with 41.6% of rural veterans (963 of 2,316) vs. 45.2% of nonrural veterans (4,110 of 9,086) (adjusted odds ratio: 0.88; 95% confidence interval: 0.73-1.04) having annual repeat screening in the expanded 31-day to 18-month window.
“Among a national cohort of veterans, rural residence was associated with numerically lower odds of annual repeat lung cancer screening than nonrural residence,” the authors concluded. “Continued, intentional outreach efforts to increase annual repeat lung cancer screening among rural veterans may offer an opportunity to decrease deaths from lung cancer.”
The authors pointed out that “Barriers to cancer care for rural populations include lower socioeconomic status, lack of geographic access to screening services and specialty care and inadequate provider-patient communication. Veterans face additional barriers to care, such as limited access to affordable and convenient healthcare, concerns about social exclusion and stigma and unmet basic needs for self and family, that may prevent them from pursuing health-seeking behavior such as lung cancer screening. Although U.S. policies are supportive of annual screening for individuals at a high risk for lung cancer, these barriers may reduce appropriate repeat lung cancer screening examinations for rural dwellers.”
Researchers emphasized the importance of increasing uptake of annual repeat lung cancer screening for rural veterans as a way to decrease the number of deaths from lung cancer, the leading cause of cancer deaths in the United States.
“Rural veterans have lower odds of both undergoing initial lung cancer screening and pursuing annual repeat lung cancer screening than their nonrural counterparts,” they advised. “Future interventions should specifically focus on gathering data on barriers to lung cancer screening for veterans through the collection of qualitative data and developing strategies to increase rural veterans’ uptake of initial and annual repeat lung cancer screening.”
- Spalluto LB, Lewis JA, Samuels LR, Callaway-Lane C, et. al. Association of Rurality With Annual Repeat Lung Cancer Screening in the Veterans Health Administration. J Am Coll Radiol. 2022 Jan;19(1 Pt B):131-138. doi: 10.1016/j.jacr.2021.08.027. PMID: 35033300.

