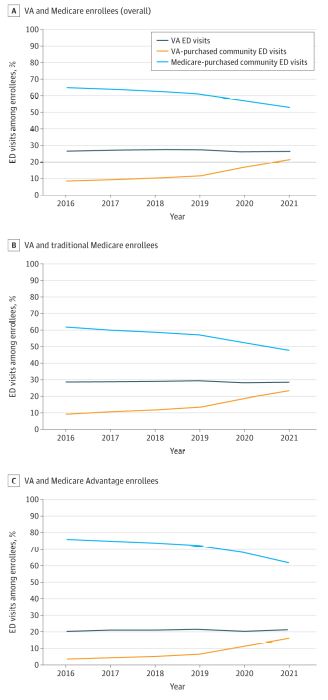
Click to Enlarge: Proportion of Emergency Department (ED) Visits Paid by the US Department of Veterans Affairs (VA) and by Medicare, Overall and Stratified by Traditional Medicare vs Medicare Advantage From 2016 to 2021All individuals were enrolled in the VA and either traditional Medicare or Medicare Advantage. Inpatient and outpatient ED visits were identified using VA data as well as traditional Medicare and Medicare Advantage claims. Source: JAMA Network
BOSTON — At least $2 billion of VA spending for community emergency department care in 2021 was due to a payer shift from Medicare, according to a recent research letter.
The researcher published in JAMA Health Forum determined that, between 2016 and 2021, the percentage of VA-purchased community ED visits increased from 8.0% to 21.1%, while Medicare-purchased community ED visits decreased from 65.2% to 52.6%.1
The patterns were similar among veterans enrolled in traditional Medicare (TM) and Medicare Advantage (MA), according to the authors from Beth Israel Deaconess Medical Center at Harvard Medical School, the Harvard T.H. Chan School of Public Health, the Boston VA Healthcare System and the Boston University School of Public Health.
“When stratifying by site and payer, VA-purchased community ED visits increased 172.7% from 66 per 1,000 veterans in 2016 to 180 per 1,000 veterans in 2021,” they wrote. “Medicare-purchased community ED visits were increasing pre-MISSION Act implementation but decreased 17.9% from 546 per 1,000 veterans in 2018 to 448 per 1,000 veterans in 2021. The percentage of all VA ED visits remained stable from 26.8% in 2016 to 26.3% in 2021.”
In 2018, the research letter pointed out, the U.S. Congress enacted the Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act, broadening veterans’ access to community care. “Since its 2019 implementation, there has been a marked increase in community emergency department (ED) visits paid by the US Department of Veterans Affairs (VA) and in VA spending on community ED care,” according to the study team. “An important dynamic arises among veterans eligible for VA coverage (eg, due to service-connected disability) and also enrolled in Medicare. Given that community care can be paid by the VA or Medicare, there is potential for payer substitution or cost shifting for ED care from Medicare to the VA. Understanding changes in ED payer source post–MISSION Act implementation is critical to inform national efforts to improve health care delivery for veterans and ensure optimal use of federal funds.”
The researchers used linked Medicare-VA data between Jan. 1, 2016, and Dec. 31, 2021, to identify adult veterans covered by both programs. From the Program Integrity Tools database, the number of VA ED visits at VA or community facilities purchased by the VA were obtained. Using ED revenue center codes from traditional Medicare (TM) and Medicare Advantage (MA) data, the investigators identified Medicare-purchased community ED visits and calculated the number of yearly ED visits per 1,000 veterans in Medicare overall and by VA ED visits, VA-purchased community ED visits and Medicare-purchased community ED visits. The study also determined the yearly percentage of ED visits across those three 3 categories and estimated total costs shifted from Medicare to VA post-MISSION Act implementation. Data analysis was performed from Feb. 1, 2023, to Sept. 18, 2024.
Of the nearly 5 million VA and Medicare enrollees in 2016 and about 4.8 million in 2021–95.6% male, mean age 74—the percentage with at least 1 ED visit was 37.0% in 2016 and 37.6% in 2021. “ED visits increased 8.0% from 820 per 1,000 veterans in 2016 to 886 per 1,000 veterans in 2019,” the study noted. “In 2020, during the COVID-19 pandemic, ED visits decreased to 769 per 1,000 veterans but increased to 852 per 1,000 veterans in 2021.”
Decrease in Medicare ED Spending
Results found that, between 2016 and 2021, there was a notable decrease in Medicare-purchased community ED visits and a concomitant increase in VA-purchased community ED visits. “Results suggest a substitution effect and cost-shifting from Medicare to VA following MISSION Act implementation, which we estimated as approximately $2 billion in 2021,” the authors explained. “This shift is particularly concerning among veterans enrolled in MA, since plans receive capitate payments regardless of actual use of VA- or Medicare-covered services. Policymakers and VA leaders should consider health reforms to improve care efficiency for veterans.”
The researchers added, “This study’s observational design limited our ability to infer causality between MISSION Act implementation and payer change. Nevertheless, using comprehensive data on Medicare and VA enrollees, this study showed that costs of community ED care for veterans are shifting from Medicare to the VA.”
An article from the VA Palo Alto, CA, Healthcare System and Stanford University appeared last March in JAMA Network Open and put a spotlight on the dramatic increase in veterans’ use of non-VA emergency care.2
That study used VA data from more than 19 million ED visits during FY 2016-2022 to examine national trends in the frequency and types of community ED visits and to explore the association between VA facilities’ purchase of community care and facility and regional factors. Of 19,787,056 ED visits from FY 2016-22, the majority (73%) occurred at VA facilities.
The researchers found that:
- The annual number of community ED visits increased 154% from FY 2016 to 2022, while the number of unique users of community emergency care increased by 134%. The proportion of all ED visits that occurred in the community progressively increased from 18% in FY 2016 to 37% in FY 2022.
- Total community care ED payments, adjusted to 2021 dollars, were $1.18 billion in FY 2016. By FY 2022, VA paid approximately $6.15 billion for community ED care.
- The most-common reasons for community ED visits were chest pain (6%), abdominal pain (3%) and serious bloodstream infection (3%). The costliest conditions treated in community EDs during the study period were septicemia, acute myocardial infarction and COVID-19.
- The average proportion of ED visits purchased by a VA facility increased from 14% in FY 2016 to 32% by FY 2022.
- Low-complexity VA facilities were more likely to purchase community emergency care than their high-complexity counterparts.
“Emergency care now encompasses over one-third of the total community care expenditure,” the researchers wrote. “This underscores the urgency of addressing the underlying factors contributing to this budgetary surge and seeking solutions for a potentially unsustainable trend. The pronounced shift toward community ED care highlights the need for policies that minimize fragmented patient experiences across care settings and navigate the complexities of providing and purchasing community emergency care.”
- Burke LG, Ma Y, Phelan J, et al. Cost Shifting for Emergency Care of Veterans With Medicare After MISSION Act Implementation. JAMA Health Forum. 2024;5(12):e244312. doi:10.1001/jamahealthforum.2024.4312
- Vashi AA, Urech T, Wu S, Tran LD. Community Emergency Care Use by Veterans in an Era of Expanding Choice. JAMA Netw Open. 2024 Mar 4;7(3):e241626. doi: 10.1001/jamanetworkopen.2024.1626. PMID: 38457180; PMCID: PMC10924239.


