WASHINGTON, DC — The VA had received over 700,000 PACT Act-related claims as of last month, testing the department’s processing capacity and threatening to significantly increase the existing backlog of claims.
In June, the backlog—defined as claims that have taken longer than 125 days to complete—stood at approximately 227,000. The Veterans Benefits Administration (VBA) predicted that number will approach 400,000 by 2024.
As part of the PACT Act, VBA was required to present Congress with a long-term modernization plan, which they did in March. The plan includes the piloting of automation technology that, once rolled out systemwide, will help bring the backlog down to manageable numbers. Legislators questioned whether the current automation plans would be comprehensive or swift enough to make a difference before the backlog significantly impacts veterans, however.
“Modernization may not be able to meaningfully reduce the backlog until two years from now,” noted House VA Subcommittee Chair Morgan Luttrell (R-TX) at a hearing earlier this summer. “However, some veterans don’t have two years to wait for this technology.”
“[Veterans] are struggling with 1950s-era procedures and a hodgepodge of dysfunctional IT systems,” added Rep. Matt Rosendale (R-MT). “The [Veterans Benefits Management System] is barely 10 years old but needs substantial upgrades to meet veterans’ needs.”
Through the first decade of the 21st century, the veterans’ benefits system remained mostly paper-based. This antiquated system, combined with an influx of new veterans who served in Iraq and Afghanistan, resulted in a crisis point around 2010. Reports of a massive backlog of claims began gaining national attention. In VBA facilities, paper files were photographed stacked in towers on the floor. In one facility, the floor was threatening to collapse under the weight of all the paper.
In 2013, VBA rolled out its electronic Veterans Benefits Management System (VBMS) and began digitizing the paper records, which also sped up the benefits process as a whole. The backlog peaked in 2014 at more than 600,000 claims but was eventually whittled down to approximately to 68,000 in 2019.
That VBMS now is a decade old and starting to show its age.
“The system crashes or often requires rebooting,” explained David Bump, who was testifying on behalf of the American Federation of Government Employees (AFGE) and is a 21-year employee of VBA. “Claims processors justifiably fear when the system goes down that they may suffer consequences to their performance metrics through no fault of their own.”
While VA officials made no promises that automation would address the sluggishness of the system as a whole, they did promise that it would speed up VBA processors’ jobs completing individual claims.
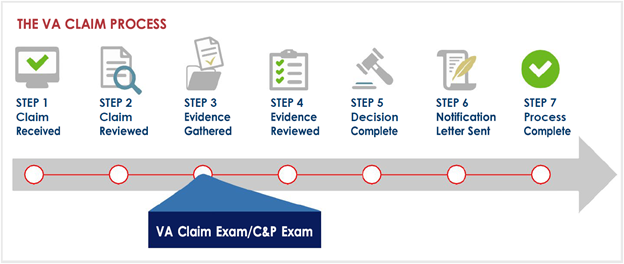
“In 2021, VBA established a proof of concept for automated decision support (ADS),” explained Acting Assistant Deputy Undersecretary Raymond Tellez. “ADS leverages technology to automate tasks in the claims process to determine eligibility, gathering evidence and auto-ordering an exam when necessary.”
Specifically, ADS takes diagnostic codes, such as for sleep apnea or asthma, both of which were added to the prototype earlier in its development, and scans through patient records for data related to that condition. VBA had planned to add a handful of diagnostic codes to the system every quarter but, following the passage of the PACT Act, moved to add the 26 presumptive conditions covered under the legislation.
At the top of the list is hypertensive vascular disease, which accounts for approximately 117,000 of the existing claims submitted under the PACT Act. Next on the list is allergic rhinitis (72,000), followed by maxillary sinusitis (34,000) and bronchial asthma (31,000).
To accomplish this kind of automation on a larger scale, VBA will need to do more work on the front end, Tellez explained.
“The first thing we’re addressing is our corporate database, which has all of the data around the benefits claims, rating and historical data,” he said. “That is a monolithic database that is not structured properly to enable [this]. Our first activity is updating this massive database to make it more accessible.”
Asked as a VBA employee where he would like to see the department focus, Bump said that automation of data scanning is fine, but that finding ways to get those files to VBA sooner should also be on the department’s radar.
“If we could get to a point where we didn’t have to request that [medical] information; whereas soon as a veteran filed a claim or as soon as they were discharged that data was already there, that would be great,” he said. “Right now, we have to go and make requests to [to DoD]. If we didn’t have to request those things. If it was already provided, that would reduce the development time. That would reduce the backlog. Some of those records you can get in less than a day, but many you can’t. If we would think about those things instead of technical requirements, I think we’d be a lot further in the process.”
- VA Benefits Claim Exam Information, https://www.benefits.va.gov/COMPENSATION/claimexam.asp