Only 15.3% of Eligible Patients Received All Interventions
INDIANAPOLIS — Meticulously following clinical guidelines in VA patients who suffered transient ischemic attack or nonsevere ischemic stroke reduced by nearly one-third their risk of death within a year, according to a new study.
In the cohort study led by researchers at Richard L. Roudebush VAMC, of 8,076 patients with those cardiovascular events from October 2010 until September 2011, only 15.3% were recipients of so-called without-fail care.1
That was defined as receiving all guideline-concordant processes of care for which they were eligible:
-
brain imaging,
-
carotid artery imaging,
-
antihypertensive intensification,
-
high- or moderate-potency statin therapy,
-
anti-thrombotics, and
-
anticoagulation for atrial fibrillation.
The study team concluded that receiving all six processes was associated with a 31.2% reduction in mortality at one year. The intensive care did not lower risk of recurrent stroke, however.
“Widespread implementation of these processes should be strongly considered for patients with TIA and non-severe ischemic stroke,” wrote study authors, which also included representatives from VAMCs in Los Angeles, Omaha, NB, and West Haven, CT. “In addition, health care systems should consider routinely measuring key processes of care for patients with TIA in addition to the quality measurement that exists for patients with stroke.”
The research team emphasized, “Clinicians should ensure that patients with transient ischemic attack and non-severe ischemic stroke receive all guideline-concordant processes of care for which they are eligible.”
The study, published online recently by JAMA Network Open, noted that early evaluation and management of patients with TIA and nonsevere ischemic stroke improves outcomes but that there was a need to identify processes of care associated with reduced risk of death or recurrent stroke among those patients. Included in the analysis were all patients with TIA or non-severe ischemic stroke at VA emergency department or inpatient settings during that time period. Data was analyzed from March 2018 to April 2019.
“Patients with transient ischemic attack and nonsevere ischemic stroke are at high risk of recurrent vascular events,” study authors explained. “However, studies have demonstrated that timely delivery of guideline-concordant care can dramatically reduce this risk.4–7 Studies reporting risk reductions of at least 70% for recurrent events among patients with TIA or nonsevere ischemic stroke have emphasized early evaluation and management; however, these studies differed in terms of the processes of care that were provided.4-8 The American Heart Association/American Stroke Association stroke prevention guidelines recommend a broad range of processes, including diagnostic processes (e.g., brain imaging) and secondary prevention interventions (e.g., hypertension management).”
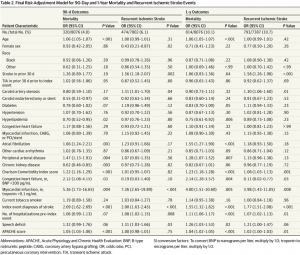
During review, the authors calculated risk of all-cause mortality and recurrent ischemic stroke at 90 days and one year while also examining 28 processes of care to determine which were essential.
Participants were veterans who had either TIA or nonsevere stroke. Their mean age was 67.8; 96% were male, and 73.4% were white.
Results indicate that 474 of the patients had a recurrent ischemic stroke within 90 days, and 793 (10.7%) had a recurrent ischemic stroke within a year. In terms of mortality, 320 (4.0%) died within 90 days, and 814 (10.1%) died within one year.
Continue Reading: