Study Recommends More of That Information Be Included in VA EHR
 DURHAM, NC — Awareness is growing that social and behavioral determinants of health (SDH)—essentially personal circumstances and environmental factors that shape conditions of daily life—have a significant effect on clinical and economic outcomes.
DURHAM, NC — Awareness is growing that social and behavioral determinants of health (SDH)—essentially personal circumstances and environmental factors that shape conditions of daily life—have a significant effect on clinical and economic outcomes.
Among the questions raised is whether adding patient-reported SDHs to a model that is based on electronic health record (EHR) data could be used to better estimate risk of future hospitalization.
A study in JAMA Network Open suggested that can be case, especially at the VA, explaining, “From a societal perspective, addressing SDH factors could increase the effectiveness of prevention and treatment efforts, health care use, and health expenditures. Clinician recognition of patients’ SDH vulnerabilities creates opportunities to offer social service referrals and targeted interventions for high-risk patients.”1
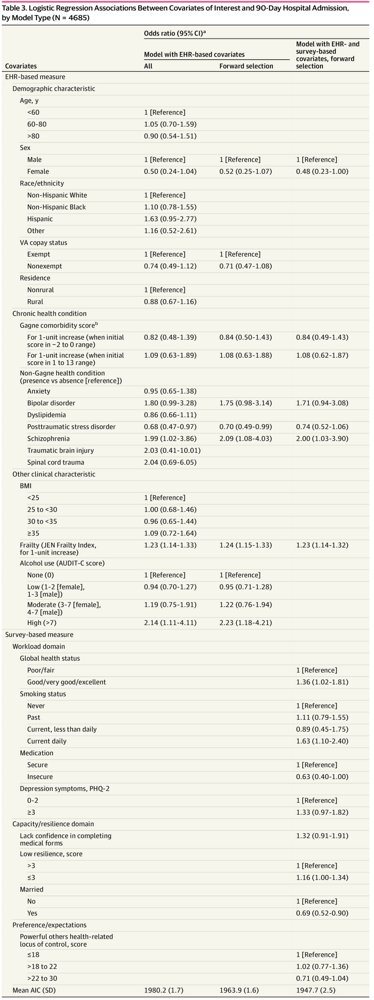
A survey study of 4,685 veterans with one-year risk in the 75th percentile or higher for hospitalization or death was used to reach those conclusions. Researchers from the Center for Health Services Research in Primary Care at the Durham, NC, Veterans Affairs Health Care System reported that a logistic regression model that included patient-reported social determinants of health outperformed a logistic model that was based only on EHR variables.
The authors pointed out that, while the association between individual SDH is acknowledged, not enough is known about the value of social issues in explaining variation in outcomes for high-risk patients. That’s why they conducted a study to both describe SDH factors among veterans who are at high risk for hospitalization and to determine whether adding patient-reported SDH measures to EHR measures would improve predictions of 90-day and 180-day all-cause hospital admission.
As part of the research, a survey was mailed between April 16 and June 29, 2018, to a nationally representative sample of 10 000 VA patients at higher one-year risk of hospitalization or death, based on a VA EHR-derived risk score. Included in the survey were multiple SDH measures such as resilience, social support, health literacy, smoking status, transportation barriers and recent life stressors. Responses were received from 4,685 patients, for a response rate of 46.9%.
The study team compared the EHR-based characteristics of survey respondents and nonrespondents using standardized differences. Specifically, estimation of 90-day and 180-day hospital admission risk was assessed for three logistic regression models:
- A base model of all prespecified EHR-based covariates,
- A restricted model of EHR-based covariates chosen via forward selection based on minimizing Akaike information criterion (AIC), and
- A model of EHR- and survey-based covariates chosen via forward selection based on AIC minimization.
Results suggested that respondents were comparable to nonrespondents in most characteristics, although survey respondents tended to be older, e.g. , >80 years old, 881 [18.8%] vs. 800 [15.1%]), included a higher percentage of men (4,391 [93.7%] vs. 4,794 [90.2%]), and were composed of more white non-Hispanic veterans (3,366 [71.8%] vs 3,259 [61.3%]).
Based on Akaike information criterion, the regression model with survey-based covariates and EHR-based covariates was found to better estimate hospital admission at 90 days (AIC, 1947.7) and 180 days (AIC, 2951.9) than restricted models with only EHR-based covariates (AIC, 1980.2 at 90 days; AIC, 2981.9 at 180 days). “This result was due to inclusion of self-reported measures such as marital or partner status, health-related locus of control, resilience, smoking status, health literacy, and medication insecurity,” researchers explained.
The study concluded that bolstering EHR data with patient-reported social information improved estimation of 90-day and 180-day hospitalization risk, while also putting a spotlight on specific SDH factors that might identify individuals who are at high risk for hospitalization.
Prevention Effectiveness
“From a societal perspective, addressing SDH factors could increase the effectiveness of prevention and treatment efforts, health care use, and health expenditures. Clinician recognition of patients’ SDH vulnerabilities creates opportunities to offer social service referrals and targeted interventions for high-risk patients,” the study pointed out.
Background information in the report noted that, in 2014, the Health and Medicine Division of the Institute of Medicine proposed that a battery of SDH measures be universally incorporated into EHRs in an “interoperable fashion.”
The Department of Health and Human Services reaffirmed the recommendation after an analysis found that Medicare beneficiaries with social risk factors had worse outcomes than beneficiaries without them. At the same time, a National Academies of Sciences, Engineering, and Medicine panel recommended identification and incorporation of a core set of SDH factors into federal payment reforms.
“Because SDH measures are not routinely captured in most EHRs in general, little is known about which specific factors are most predictive of acute care use, such as hospitalization,” the authors advised. “Studies have found associations between hospitalizations and factors such as neighborhood socioeconomic status, race/ethnicity, food insecurity and social isolation, but little is known about other social and behavioral characteristics, such as resilience and health-related locus of control.”
That history has special relevance in the VA healthcare system because of a long-standing mission to address SDH factors in its patient population. In addition, beneficiaries of VA healthcare generally have greater medical, social and behavioral complexity than nonveterans or veterans not enrolled in that healthcare system.
“With 2 decades of experience with a national EHR for millions of patients in the nation’s largest integrated health system, the VA is well positioned to inform selection and integration of SDH measures into EHRs,” according to the researchers.
The study recommended adding certain SDH factors to a commonly used list. “One of the measures that improved estimates of hospitalization in our models (smoking status) is in the list recommended by the National Academy of Medicine,” the authors pointed out. “Our findings suggest that adding factors such as physical function, marital or partner status, and medication insecurity to annual preventive health screenings could offer an opportunity to improve prediction algorithms. Routine collection of these risk factors would enable the VA to flag patients at heightened risk for hospitalization due to these factors and enable EHR-based alerts for clinicians about individuals who need supportive services. Incorporating these types of factors into the EHR could also assist with population management and health system decisions, for example by highlighting the need for partnerships with certain community agencies.”
- Zulman DM, Maciejewski ML, Grubber JM, et al. Patient-Reported Social and Behavioral Determinants of Health and Estimated Risk of Hospitalization in High-Risk Veterans Affairs Patients. JAMA Netw Open. 2020;3(10):e2021457. Published 2020 Oct 1. doi:10.1001/jamanetworkopen.2020.21457

