Quality, Safety Compared to Women’s Care at Private Sector Facilities
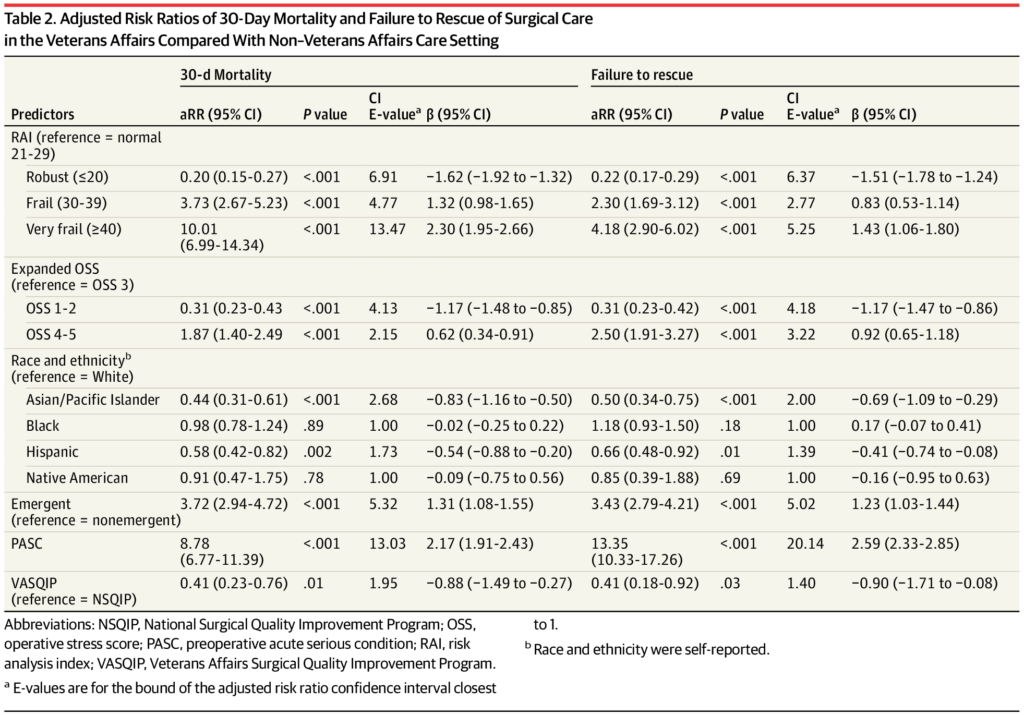
Adjusted Risk Ratios of 30-Day Mortality and Failure to Rescue of Surgical Care in the Veterans Affairs Compared With Non–Veterans Affairs Care Setting Abbreviations: NSQIP, National Surgical Quality Improvement Program; OSS, operative stress score; PASC, preoperative acute serious condition; RAI, risk analysis index; VASQIP, Veterans Affairs Surgical Quality Improvement Program.
a. E-values are for the bound of the adjusted risk ratio confidence interval closest to 1.
b. Race and ethnicity were self-reported. Source: JAMA Network Open
PALO ALTO, CA — Only 11% of U.S. military veterans are women, according to recent statistics, and they make up even a smaller percentage of patients using VA healthcare—about 10%.
Yet, a new national cohort study found that VA surgical care provided to women veterans was associated with half the risk of surgical mortality and failure to rescue compared with women’s private-sector surgical care.
The authors from Stanford University School of Medicine and the VA Palo Alto, CA, Healthcare System said their findings suggested that VA hospitals might be better equipped to care for the unique perioperative needs and risk profiles of veterans, regardless of sex. The results were published in JAMA Surgery.1
Women are the fastest growing group of using VHA services, having tripled since 2001 from 159,810 patients to more than 600,000 in 2023. They make up 30% of all new VHA patients.
“Recent legislation facilitates veterans’ ability to receive non-Veterans Affairs (VA) surgical care,” the authors wrote. “Although veterans are predominantly male, the number of women receiving care within the VA has nearly doubled to 10% over the past decade, and recent data comparing the surgical care of women in VA and non-VA care settings are lacking.”
In response, the study team sought to compare postoperative outcomes among women treated in VA hospitals vs. private-sector hospitals.
Their coarsened exact-matched cohort study across nine noncardiac specialties in the VA Surgical Quality Improvement Program (VASQIP) and American College of Surgeons National Surgical Quality Improvement Program (NSQIP) took place from Jan. 1, 2016, to Dec. 31, 2019, with data analysis in January 2023.
The participants were adult female patients receiving surgical care in VA or private-sector hospitals. The researchers calculated postoperative 30-day mortality and failure to rescue (FTR).
Among 1.9 million procedures analyzed, patients in VASQIP were younger (VASQIP: mean age, 49.8 [SD, 13.0] years compared to NSQIP: mean age, 55.9 [SD, 16.9] years; P <0 .001). Although most patients in both groups identified as white, there were significantly more Black women in VASQIP compared with NSQIP (29.6% vs. 12.7%; P < 0.001).
The results indicated that the mean risk analysis index score was lower in VASQIP (13.9 [SD, 6.4]) compared with NSQIP (16.3 [SD, 7.8]) (P < 0.001 for both). Patients in the VA were more likely to have a preoperative acute serious condition (2.4% vs. 1.8%: P <0 .001), but cases in NSQIP were more frequently emergent (6.9% vs. 2.6%; P < 0.001).
The researchers reported that the 30-day mortality, complications and FTR were 0.2%, 3.2% and 0.1% in VASQIP (n = 36,762 procedures), compared with 0.8%, 5.0% and 0.5% in NSQIP (n = 1,876,271 procedures), respectively (all P <0 .001). Among about 1.8 million matched women (n = 36,478 procedures in VASQIP; n = 1,727,062 procedures in NSQIP), the rates were 0.3%, 3.7% and 0.2% in NSQIP and 0.1%, 3.4% and 0.1% in VASQIP (all P < 0.01).
Lower Risk of Death
“Relative to private-sector care, VA surgical care was associated with a lower risk of death (adjusted risk ratio [aRR], 0.41; 95% CI, 0.23-0.76,” the authors pointed out. “This finding was robust among women undergoing gynecologic surgery, inpatient surgery, and low-physiologic stress procedures. VA surgical care was also associated with lower risk of FTR (aRR, 0.41; 95% CI, 0.18-0.92) for frail or Black women and inpatient and low-physiologic stress procedures.”
The study team concluded that, although women comprise the minority of veterans receiving care within the VHA, VA surgical care for women in this study “was associated with half the risk of postoperative death and FTR. The VA appears better equipped to meet the unique surgical needs and risk profiles of veterans, regardless of sex, and health policy decisions, including funding, should reflect these important outcome differences.”
Background information in the article noted that the VHA provides care to more than 9 million veterans across the United States and is the nation’s largest integrated health care system. Because of concerns regarding the timeliness and quality of care in VHA, the U.S. Congress passed the Veterans Access, Choice and Accountability Act (i.e. the Veterans’ Choice Program or the Choice Act) and subsequently the Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act to increase veterans’ private-sector care access.
“While a primary goal of the MISSION Act is to improve veterans’ timely access to needed health care services, the success of this legislation in achieving this goal is predicated on the assumption that private-sector care is equal or better than care rendered by the VA, which is not clearly supported by existing clinical or survey data,” the study suggested.
As for surgical care, surgical care, several studies indicated that VA surgical-care quality is comparable with, and often better, than that provided in the private-sector. “Our group recently compared postoperative outcomes among veterans treated in VA hospitals vs. patients in private-sector hospitals and found the risk of 30-day mortality was approximately 40% lower for VA surgical care,” the researchers pointed out. “However, an important limitation of this prior work was the predominantly male composition of the veteran sample. As such, comparisons focused on surgical care in women may not have been adequately assessed.”
The report also advised that, although veterans are predominantly male, the number of women receiving care within the VA has nearly doubled to 10% over the past decade and is projected to continue growing.
“Despite women representing a minority of veterans and having unique health needs requiring subspecialty care, in this study, postoperative mortality and FTR for women was significantly lower in VA compared with private-sector hospitals,” the authors explained. “ In combination with prior work, these findings challenge the assumption that shifting care to the private sector can improve timeliness of surgical care without diminishing its quality.”
According to the VSO Disabled American Veterans, 63% of women veteran patients in VHA have a service-connected disability. Many have complex health care needs and are eligible for a lifetime of treatment, readjustment services, disability compensation, education and other VA benefits, according to the group.
The study team also advised that veterans are “a unique patient population that benefits from the tailored care processes and resources the VHA has developed, which are not and cannot be offered to the same extent or availability in the private sector. Furthermore, these VHA systems could be at risk should private-sector diversion through community care programs continue to reduce VHA utilization and funding. Future decisions regarding care setting at both the individual patient level and the congressional level should reflect these important differences in the quality and safety of surgical care.”
- George EL, Jacobs MA, Reitz KM, et al. Outcomes of Women Undergoing Noncardiac Surgery in Veterans Affairs Compared With Non–Veterans Affairs Care Settings. JAMA Surg. Published online February 28, 2024. doi:10.1001/jamasurg.2023.8081

