BEDFORD, MA — When initiating gender-affirming hormone therapy (GAHT) at the VHA, clinicians achieved high overall concordance between current GAHT initiation practices and guidelines, particularly for feminizing GAHT, according to a recent study.
The study published in Frontiers of Endocrinology assessed guideline concordance around feminizing and masculinizing GAHT initiation in the VHA. Study authors are affiliated with VA healthcare systems in Bedford, MA; Pittsburgh; West Haven, CT; Boston and the VA’s Office of Patient Care Services in Washington, DC.1
GAHT is a “common medical intervention sought by transgender and gender diverse individuals, who often experience gender dysphoria, an incongruence between one’s gender identity and sex assigned at birth that results in clinically significant distress or impairment,” study authors explained. “To alleviate gender dysphoria among transgender and gender diverse individuals, evidence-based treatments include feminization or masculinization through interventions, such as GAHT, one of the most utilized gender-affirming medical interventions.”
The authors noted that studies have found that the treatment can improve mental health and quality of life and lower the risk for suicidal ideation and suicide attempts among transgender and gender-diverse veterans, as well as others.
Initiating GAHT in line with clinical guideline recommendations “ensures delivery of high-quality care, but no previous studies have examined how current GAHT initiation compares to recommended GAHT initiation,” they pointed out.
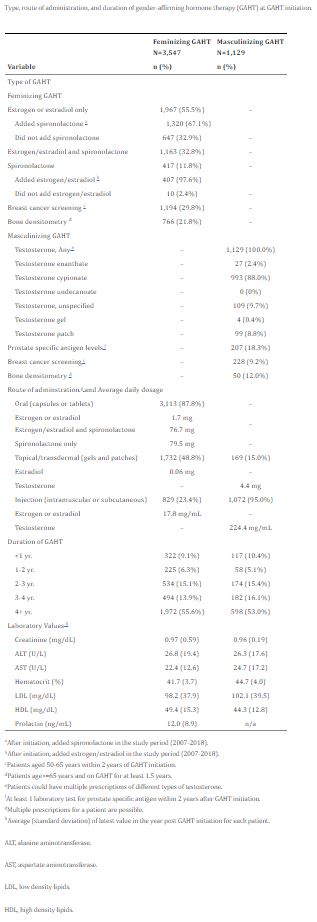
To remedy that, the study team used outpatient and inpatient data from VHA’s Corporate Data Warehouse. The study participants included 4,676 veterans with a gender identity disorder diagnosis—3,547 seeking feminization and 1,229 seeking masculinization—between 2007 and 2018 in VHA. The authors assessed demographics and health conditions of veterans seeking GAHT, as well as the proportion of clinical efforts that were concordant with six VHA guidelines on feminizing and masculinizing GAHT initiation.
Overall, the results indicated that there was “high concordance between current GAHT initiation practices in VHA and guidelines. In particular, VHA clinicians initiated feminizing GAHT in concordance with clinical guidelines.”
When compared to veterans who received masculinizing GAHT, “a higher proportion of veterans who received feminizing GAHT were older (≥60 years: 23.7% vs. 6.3%), white non-Hispanic (83.5% vs. 57.6%), and had a higher number of comorbidities (≥7: 14.0% vs. 10.6%),” study authors reported.
The authors found that a higher proportion of veterans receiving masculinizing GAHT were Black non-Hispanic (21.5% vs. 3.5%), had posttraumatic stress disorder (43.0% vs. 33.9%) and had experienced military sexual trauma (33.5% vs.16.8%) than veterans receiving feminizing GAHT.
Guideline-Concordance High
In veterans who started feminizing GAHT with estrogen, 97.0% were found to be “guideline-concordant due to no records of contraindication, including venous thromboembolism, breast cancer, stroke or myocardial infarction. Among veterans who started spironolactone as part of feminizing GAHT, 98.1% were guideline-concordant since they had no records of contraindication, including hyperkalemia or acute renal failure,” the researchers reported.
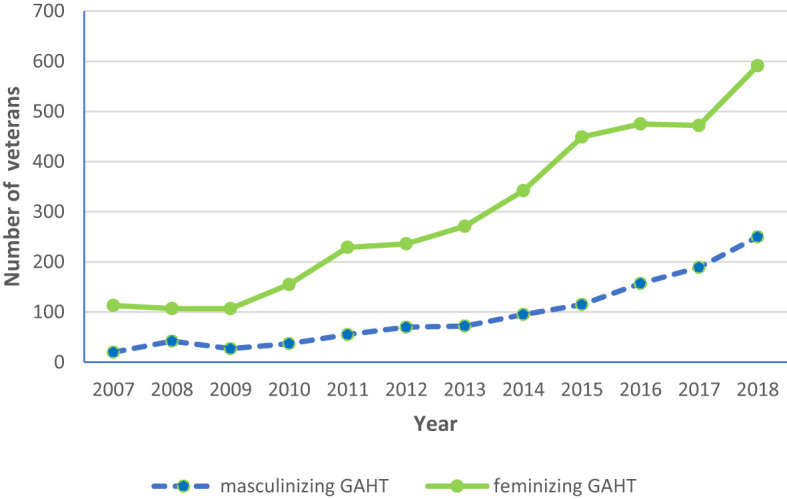
Click to Enlarge: Longitudinal trends in the number of veterans on feminizing and masculinizing gender-affirming hormone therapy (GAHT) (2007–18).
Source: Frontiers in Endocrinology
In veterans starting masculinizing GAHT, 90.1% were determined to be guideline-concordant due to no documentation of contraindications, such as breast or prostate cancer. Furthermore, hematocrit was measured in 91.8% of veterans before initiating masculinizing GAHT, and 96.5% of these veterans didn’t have an elevated hematocrit (>50%) prior to starting masculinizing the process, the researchers pointed out. In addition, the authors discovered that, “among veterans initiating feminizing and masculinizing GAHT, 91.2% had documentation of a gender identity disorder diagnosis prior to treatment initiation.”
Understanding the level of quality of care is important to prevent adverse health outcomes at GAHT initiation in transgender and gender diverse individuals, the authors advised, adding that future research is needed to “examine predictors of guideline discordance and health outcomes associated with guideline discordance in transgender and gender diverse veterans initiating feminizing and masculinizing GAHT. Studies are also needed to analyze guideline concordance around GAHT monitoring and management in VHA and other healthcare systems.”
Even though this study is an important first step in taking an inventory of GAHT care received by transgender and gender-diverse veterans in VHA, it had several limitations, according to the authors. Among those are using diagnosis codes instead of a patient’s self-reported gender identity, which might have biased the sample toward patients who are engaged in care and treatment. The study also didn’t capture GAHT prescriptions or care in VHA community care, which is either paid by VHA in the community or covered by non-VHA payers, such as private insurance.
The authors also pointed out that not all aspects of GAHT care are amenable to quality measures using automated data; that would include whether the patient was fully informed of risks and benefits of GAHT which would need to be assessed by chart review.
Before hormone therapy can begin, the VA requires that a diagnostic and mental health readiness evaluation must be completed by a licensed mental health provider.
The review also didn’t include any information on patients who were interested in GAHT and denied care or on gender-affirming surgery, which the VHA does not currently cover.
This spring, an advocacy group for transgender veterans filed a second lawsuit over the VA’s failure to provide or pay for gender-affirming surgeries.
The federal lawsuit was filed by the Transgender American Veterans Association, claiming the VA’s decision “amounts to discrimination on the basis of sex and transgender status” and threatens the health of veterans. Three years ago, VA Secretary Denis McDonough said the administration would move toward providing the surgeries.
Last November, McDonough said the department was still working on the change.
- Jasuja GK, Wolfe HL, Reisman JI, Vimalananda VG, et. Al. Clinicians in the Veterans Health Administration initiate gender-affirming hormone therapy in concordance with clinical guideline recommendations. Front Endocrinol (Lausanne). 2024 May 10;15:1086158. doi: 10.3389/fendo.2024.1086158. PMID: 38800485; PMCID: PMC11116601.