Military Study Blames Histologic Subtype for Most of Differences
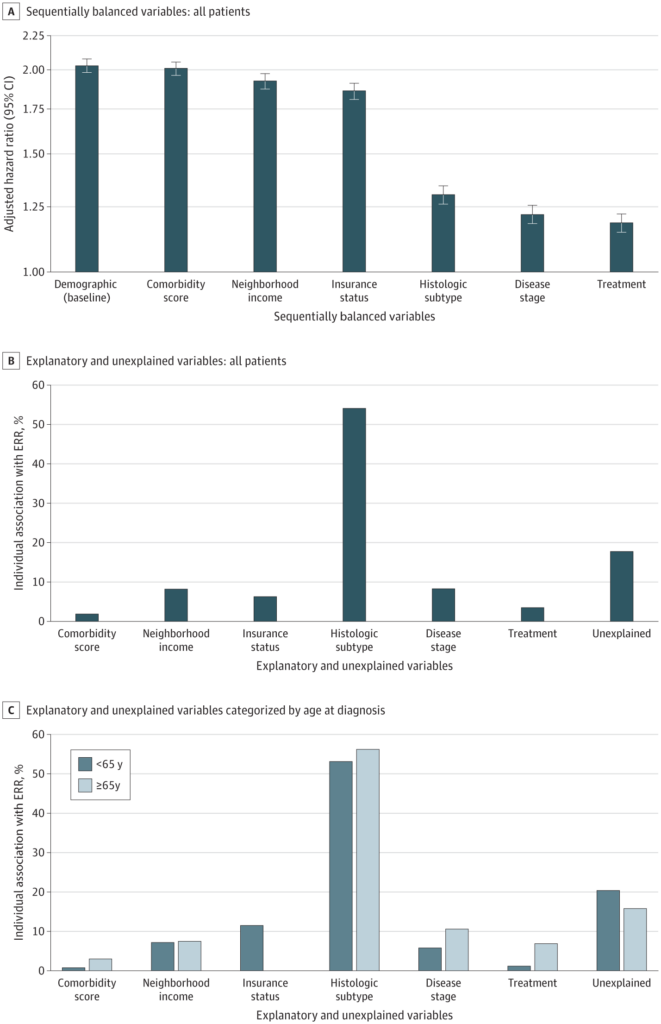
Click to Enlarge: A, Adjusted hazard ratios for risk of death for non-Hispanic Black patients compared with non-Hispanic White patients for each sequentially balanced variable. Error bars indicate 95% CIs. B, Individual associations of the explanatory and unexplained variables with the percentage ERR of death for non-Hispanic Black patients compared with non-Hispanic White patients who received a diagnosis of uterine cancer at all ages. C, Individual associations of the explanatory and unexplained variables with the percentage ERR of death for non-Hispanic Black patients compared with non-Hispanic White patients who received a diagnosis of uterine cancer at younger than 65 years vs 65 years or older.
BETHESDA, MD — Disparities in survival exist between non-Hispanic Black and non-Hispanic white patients with uterine cancer. A new study from military researchers sought to determine why.
Histologic subtype is the leading factor associated with racial survival disparity among Black and white patients with uterine cancer, and insurance status is the main modifiable factor for women younger than 65 years old, according to the recent study led by researchers from Walter Reed National Military Medical Center in Bethesda, MD.
The study published in JAMA Network Open investigated the factors most associated with racial disparities in survival between non-Hispanic Black and non-Hispanic white patients with Stage I to IV uterine cancer.1
Incidence and mortality of uterine cancer are increasing, with 66,570 new cases (including endometrial cancers and sarcomas) and 12,940 deaths estimated in the United States. Disparities in survival between non-Hispanic Black and non-Hispanic white patients with uterine cancer have endured over decades, with higher likelihoods of aggressive disease, recurrence and death among Black patients.
The factors explaining these disparities are complex, according to the authors. Differences in histologic subtype, disease stage, tumor grade, treatment, supportive services and molecular features have been connected to health disparities among patients with uterine cancer. Even among uterine cancer patients with equal access to care who receive similar treatment, racial differences in cancer diagnosis and survival still persist, the study reported.
The researchers used data from the National Cancer Database on 274,838 Black and white patients who received a diagnosis of uterine cancer from Jan. 1, 2004, to Dec. 31, 2017, with follow-up through December 2020. Statistical analysis was performed in July 2022.
The study found histologic subtype was the dominant factor associated with racial disparities in survival among Black and white patients with uterine cancer, linked to 54% of the racial disparities in survival. By age group, histologic subtype accounted for 53.1% of the total excess relative risk for patients younger than 65 years old and 56.2% of the total excess relative risk for those 65 years or older.
At the same time, insurance status was the major modifiable factor among those who received a diagnosis of uterine cancer at an age younger than 65 years, accounting for 11.5% of the excess relative risk for women younger than 65 years, according to the study.
The participants were 32,230 Black female patients (mean age at diagnosis was 63.8 years) and 242,608 white female patients (mean age at diagnosis was 63.5 years). A total of 11.7% of patients were self-described as Black, 26.2% had comorbidities, 24.5% received a diagnosis of nonendometrioid subtype, and 21.5% had Stage III to IV disease beyond the uterus.
Nonendometroid Histology
Black patients were more likely than white patients to have low income (44.1% vs. 14.0%), be uninsured (5.7% vs. 2.6%), present with nonendometrioid histologic characteristics (46.1% vs. 21.6%), have an advanced disease stage (34.1% vs. 19.8%), receive first-line chemotherapy (33.8% vs. 18.2%) and have worse five-year survival (58.6% vs. 78.5%).
Among patients who received a diagnosis at younger than 65 years of age, the hazard ratio for death for Black versus white patients was 2.43 (95% CI, 2.34-2.52) in a baseline demographic-adjusted model and 1.29 (95% CI, 1.23-1.35) after balancing other factors. Comorbidity score, neighborhood income, insurance status, histologic subtype, disease stage, treatment and unexplained factors accounted for 0.8%, 7.2%, 11.5%, 53.1%, 5.8%, 1.2% and 20.4%, respectively, of the excess relative risk among the younger Black versus white patients.
For patients 65 years or older, the hazard ratio for death for Black versus white patients was 1.87 (95% CI, 1.81-1.93) in the baseline model and 1.14 (95% CI, 1.09-1.19) after balancing other factors. Comorbidity score, neighborhood income, insurance status, histologic subtype, disease stage, treatment and unexplained factors accounted for 3.0%, 7.5%, 0.0%, 56.2%, 10.6%, 6.9% and 15.8%, respectively, of the excess relative risk among Black versus white patients aged 65 years or older.
“The results of this cohort study raise awareness of the survival disparities between Black and white patients with uterine cancer, provide insight into some of the explanatory factors, and highlight the persistent gaps in knowledge and the opportunities for further study,” the researchers concluded. “Insurance status represented an attractive modifiable factor for us to study, given how well it explained racial survival disparities among nonelderly women with breast cancer, but its association with survival among patients with uterine cancer was smaller due to the dominant role played by histologic subtype in this disease.”
They added that their data also underscored the urgency to further study the survival disparities between Black and white patients with uterine cancer associated with histologic subtype and unexplained factors, including ancestry admixture, molecular alterations, barriers to care, social determinants of health and public policy. The goal would be to achieve equity and improved outcomes.
- Kucera CW, Tian C, Tarney CM, et al. Factors Associated With Survival Disparities Between Non-Hispanic Black and White Patients With Uterine Cancer. JAMA Netw Open. 2023;6(4):e238437. doi:10.1001/jamanetworkopen.2023.8437

