WASHINGTON—With an increase in the number of servicemembers coming forward to report their experience with sexual assault during active duty, VA is slowly making progress in implementing best practices for how to evaluate and care for survivors of military sexual trauma.
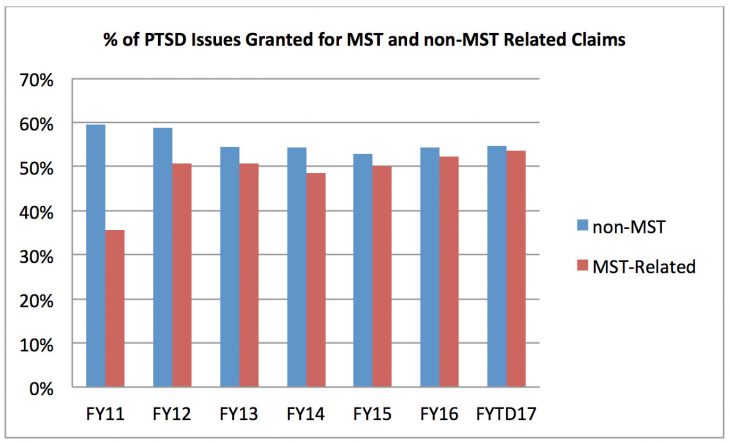
This table shows the percent of PTSD issues granted for MST-related and non-MST related claims. In FY11, there is a substantial gap: 59.5% of non-MST related PTSD claims were granted, compared to only 35.6% of MST-related PTSD claims, a nearly 24 point gap. Three years later, in FY14, the gap had shrunk to less than six points, with grant rates of 54.1% and 48.5% respectively. So far this fiscal year, the gap is only around one point, with grant rates of 54.6% for non-MST related claims and 53.4% for MST-related claims.
One of the biggest hurdles for survivors is frequently their first contact with the department—their initial evaluation. VA’s eligibility processes often require a veteran to relive specific details of their assault multiple times for VA staff whom they’ve just met. This can be retraumatizing for survivors, especially considering the goal of these meetings is to confirm the legitimacy of their claim.
“We’ve worked to fix some of these challenges. And this one in particular is like a gut punch to us,” Willie Clark Sr., VBA deputy under secretary for field operations told the House VA Oversight Subcommittee at a hearing last month. “We’ve been working providing additional training to our processors to basically say that if we can corroborate, if we can substantiate, if we can grant a claim based upon the evidence in the file, there is no need to make a call. Unfortunately what has happened is that some of our folks—and we have to get better at fixing this—they follow a checklist that says they have to call the survivor to ask these questions. We are changing these processes to put our processors in a better position. They don’t want to make these calls. It makes an individual have to relive the experiences they’ve gone through, and we have to do better at that.”
Beth Murphy, VBA’s executive director of compensation services, explained that the nature of MST claims sometimes makes it particularly difficult to avoid uncomfortable conversations with veterans. “We’re looking for a link between a diagnosed condition and an in-service event,” she explained. “What makes MST different is that it often isn’t reported in service, so we have to lean in and dig a little deeper to look for markers or indicators to signal that something may have happened. And that’s why unfortunately we have to talk to the survivor a little more and connect those dots. We do it as compassionately and sensitively as we can.”
In September 2019, VBA completed its review of approximately 9,700 previously denied MST claims from Oct. 1, 2016, through June 30, 2018. The review found that approximately 20% of the claims failed in some way to meet VBA’s requirements. After reexamining the claims, VBA sustained 900 of the denials, increased the compensation of 460, and are still developing the remaining 500.
High Compliance With MST Rules
Regarding care once veterans enter a VA facility, recent VA Inspector General evaluations show that VA is progressing in training its staff in how to best provide care for MST survivors. A review of 43 randomly selected VA facilities found high compliance with the requirements regarding MST coordinators, their activities, and the provision of care for veterans who have screened positive for MST.
The OIG found that each of the evaluated facilities had a designated MST coordinator and that 42 of 43 coordinators had generally established and monitored informational outreach activities, and 39 of 43 coordinators tracked and monitored MST-related data.
Reviewing MST-related care for 1,903 patients, evaluators found those who were referred to mental health treatment received an evaluation within one business day and a mental health diagnostic and treatment planning evaluation within 30 days of referral.
However, OIG investigators found that only 79% of MST coordinators had a process in place to communicate concerns about MST care to their facility leadership, and only 88% of leaders had a system to make sure their personnel have knowledge and skill to work with MST survivors.
This inconsistency was also reflected in the training of facility staff.
“The OIG found that of 324 clinicians hired before July 1, 2012, there were 304 (94%) who had completed MST training,” explained Julie Kroviak, MD, deputy assistant inspector general for healthcare inspections. “However, of the 529 applicable clinicians hired after July 1, 2012, only 330 (62%) had completed MST training within 90 days of entering their position. This could potentially result in newly hired clinicians providing counseling, care and service without the required MST training.”
According to veterans’ advocates, one of the most persistent barriers to female MST survivors seeking care is harassment by fellow veterans at VA facilities. Kayla Williams, senior fellow and director for military, veterans and society Programs at the Center for a New American Security, argued that VA’s End Harassment campaign should receive the level of support and leadership buy-in that the department’s suicide prevention program does.
“We should make every VA leader publicly state their commitment to ending harassment in VA facilities; take a pledge; write blogs about it; be open and transparent with their staff about how important they believe it to be. That should start with the Secretary and trickle down through all levels,” Williams declared. “It’s very important that the rate of sexual harassment and the appropriate level of response to it at VA medical centers be a part of the rating of the success of VA medical center directors. Hold them accountable for what is happening at VA facilities. If they’re not being held accountable, they will be much less likely to take it as seriously as it needs to be.”
While women are one of the fastest growing populations of veterans—and 1 in 4 women will experience sexual harassment while in uniform, compared to 1 in 100 men—nearly 40% of veterans who disclose MST to VA are men. Previous studies have shown that men submitting claims for MST-related PTSD are granted benefits at a lower rate than their female counterparts, suggesting that a cultural bias against men reporting sexual assault might be affecting the benefits process.


