Click to Enlarge: Continuation of psychiatric medications during pregnancy Source: The Journal of Maternal-Fetal & Neonatal Medicine
HOUSTON — VA medical providers and veterans need more education about the risks and benefits from continuing antidepressants during pregnancy, according to a new study.
The report in the Archives of Women’s Mental Health also suggested that awareness of alternative therapies would be valuable.1
A study team from the Baylor College of Medicine, the University of Houston and the Michael E DeBakey VA Medical Center, all in Houston, pointed out that female U.S. veterans have higher rates of mental health (MH) disorders compared to civilian females in the United States. That puts them at risk for poor MH outcomes during pregnancy.
Researchers sought to evaluate the MH burden and identify the prevalence of antidepressant prescription and discontinuation among pregnant veterans (PGVets).
To do that, they retrospectively reviewed the electronic health records (EHR) over a 2-year period of PGVets using VA maternity care benefits. Included in the study were 351 female veterans who had a current MH diagnosis of depression, anxiety or post-traumatic stress disorder (PTSD) at the onset of pregnancy.
The study team was focused on outcomes including antidepressant use prior to pregnancy, the use and discontinuation of antidepressants during pregnancy and risk factors for discontinuation.
Results indicated that PGVets had a high MH burden, with 67% of the sample having multiple comorbid diagnoses of unipolar depression, anxiety and PTSD. At the onset of pregnancy, 163 (46%) were treated with an antidepressant, the researchers explained, but only 56 (34%) continued using antidepressants through the pregnancy.
Both self-discontinuation (34%) and VA provider discontinuation (31%) of antidepressants occurred, according to the authors, who advised. “Among PGVets with documented past suicidal behaviors, 90% discontinued their active antidepressants. PGVets with indicators for more severe MH diagnoses were most likely to discontinue.”
They added, “The MH burden of PGVets and high rates of antidepressant discontinuation have implications for engaging this population in a higher level of perinatal monitoring and intervention. The findings suggest that VA providers and veterans would benefit from risks and benefits education regarding antidepressant use during pregnancy, as well as the provision of alternative therapies.”
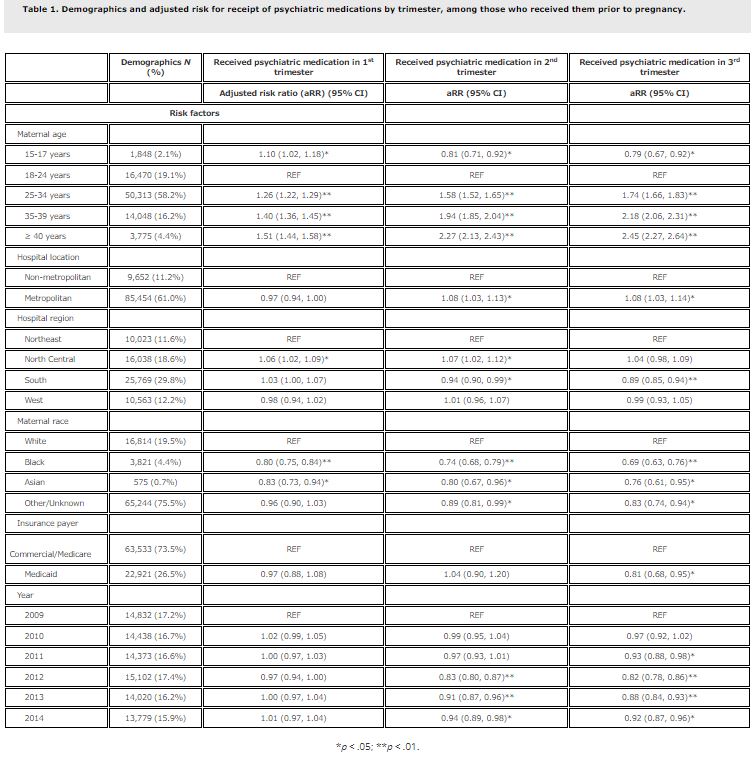
A study earlier this year, the Journal of Maternal-Fetal & Neonatal Medicine, looked at continuation of antidepressants during pregnancy in the United States overall. Researchers from the Columbia University Irving Medical Center in New York and the University of California, San Francisco used a large administrative database to determine whether psychiatric medications are continued during pregnancy and predictors of continued medication treatment.2
The study team determined that, of about 2.7 million women included in the analysis, 86,454 (3.1%) filled a prepregnancy prescription for an anxiolytic or antidepressant medication within three months of estimated conception.
Of women who filled a prepregnancy prescription, researchers reported that 49.4%, 26.1% and 20.1% filled subsequent prescriptions in the first, second and third trimesters. “Discontinuation rates ranged by pharmaceutical agent, from 16% for fluoxetine to 71% for alprazolam,” the study noted. “White women and women over 25 were more likely to continue anxiolytic and antidepressant treatment during pregnancy.”
The authors concluded, “Because untreated and under-treated mental health conditions are linked to adverse maternal outcomes, high discontinuation rates may have important implications for maternal health.”
Background information in the article noted that antidepressants and anxiolytics are among the most prescribed medications in reproductive-aged people in the United States.
“There is no consensus on optimal use of psychiatric medications in pregnancy,” according to the authors, “some women may discontinue antidepressant and anxiolytic medications when they become pregnant due to concern for birth defects and/or poor pediatric neurodevelopmental outcomes. But untreated or under-treated mental health conditions in pregnancy also carry risk for adverse maternal outcomes, including relapse of psychiatric disease and pregnancy-related death.”
The study added, “Nearly 40% of pregnancy-related deaths attributable to mental health conditions are associated with discontinuation of or change in medication treatment for a psychiatric or substance use disorder.”
Researchers suggested that large population data on continuation of antidepressants and anxiolytics could be of clinical and public health importance.
- Howard M, Ledoux T, Llaneza D, Taylor A, Sattem E, Menefee DS. Exploring the prevalence of antidepressant medication discontinuation among pregnant veterans. Arch Womens Ment Health. 2023 Sep 23. doi: 10.1007/s00737-023-01372-7. Epub ahead of print. PMID: 37740096.
- Logue TC, Wen T, Huang Y, Wright JD, D’Alton ME, Friedman AM. Continuation of psychiatric medications during pregnancy. J Matern Fetal Neonatal Med. 2023 Dec;36(1):2171288. doi: 10.1080/14767058.2023.2171288. PMID: 36710395.


