WASHINGTON—Women veterans regularly experience harassment by male veterans at VA facilities, and that harassment has a direct and lasting impact on their healthcare, VA researchers reported recently.
Investigators from the VA Greater Los Angeles Health Care System and colleagues conducted interviews with women veterans from January through March of 2015. These women all had three or more primary care encounters at a VA facility in the previous year.
One in 4 reported inappropriate comments or behavior by male veterans while they were on VA grounds, and 8% said this either usually or always occurred when at VA. These interactions included sexual and derogatory comments and questioning of the woman’s history of service and her right to care.
About two-thirds of the women interviewed screened positive for probable anxiety and military sexual trauma. Also, 80% reported combat or lifetime exposure to trauma. The women who reported harassment were less likely to report feeling welcoming at VA and more likely to report feeling unsafe and to delay or miss subsequent appointment, according to the article published in Women’s Health Issues.1
One woman told researchers that, as the only woman taking swimming therapy, she was subjected to stares and comments about women in bathing suits and subsequently quit pool therapy. Another explained that male veterans assume she’s someone’s spouse, and when she tells them she’s a veteran they tell her about how women should not be in the military.
Women account for 30% of the increase in veterans seen at VA facilities over the past five years, and the number of women using VA health services has tripled over the past 20 years. However, women still only account for about 8% of VA patients. This means that women are vastly outnumbered in most VA healthcare environments and the behavior of their male peers can have a massive impact on their experience receiving care at VA.
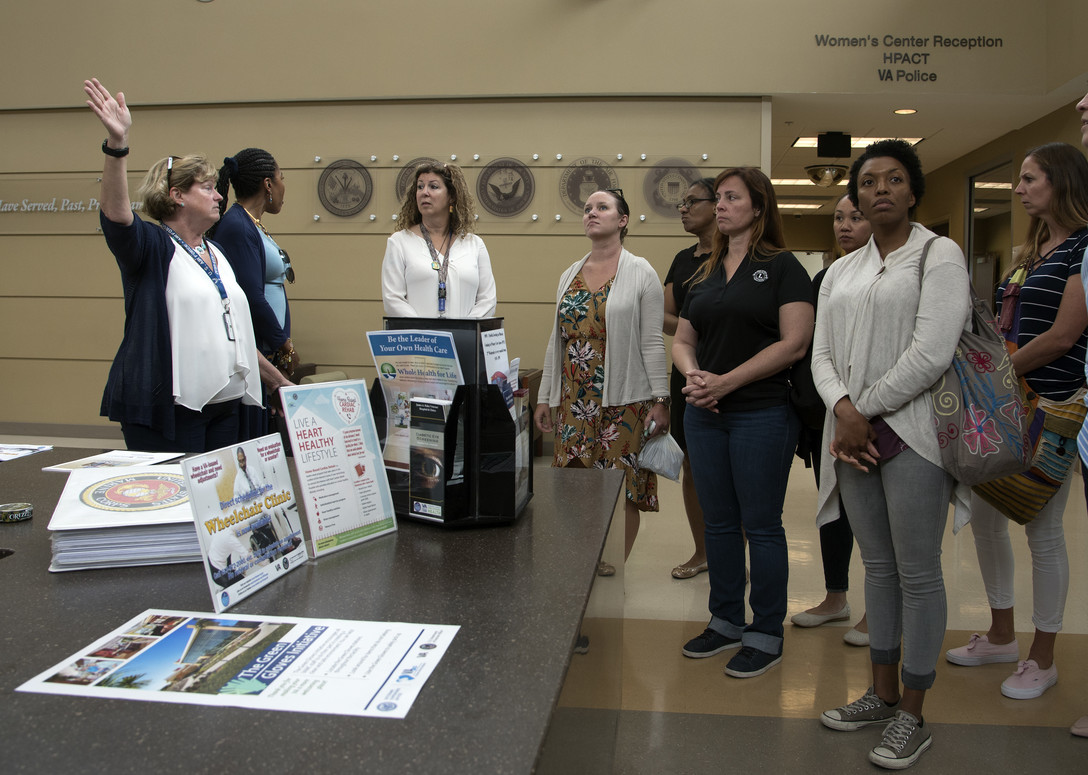
VA launched a campaign to end harassment in 2017. The department developed posters, videos and training materials and has rolled the program out to all its sites. Most of the messaging is targeted at male veterans, educating them that certain conduct is unacceptable. However, the best way to make a lasting impact on the culture might be at the local level, Patricia Hayes, PhD, VA’s Women’s Health Services Chief told the House VA Oversight Subcommittee at a hearing last month.
“The best way is for VA facilities to talk to their women veterans,” Hayes said. “I encourage facility directors to call women veterans and ask them. ‘What have you experienced at the VA? Where are the hot spots? Where are the trouble spots?’”
In the meantime, Hayes said, “we will be persistent in our culture change efforts.”
Last month’s hearing was the first House VA Committee hearing in recent memory focused solely on the health of women veterans. It came on the heels of an announcement by the committee that it was launching a bipartisan Women Veterans Task Force to help ensure equitable access to resources, benefits and care to women veterans.
“The women who serve our country are still treated as second-class servicemembers and veterans. From the long-standing prohibition barring women from combat jobs to women going into combat wearing protective equipment made for men,” declared Rep. Julia Brownley (D-CA), subcommittee chair and chairwoman of the task force. “Most troubling is the widespread incidence of sexual violence in the ranks. At least 1 in 4 servicewomen experience sexual trauma. More than half the servicemembers who report their assaults also report that their commands retaliated against them. Therefore it should not be surprising that when women leave the military, they’re reluctant to enter veteran-serving spaces [like VA].”
Meeting the Needs
Along with examining the widespread patterns of harassment at VA, the hearing looked at VA’s ability to service women’s healthcare needs. VA facilities are frequently unable to provide such basic preventive services such as Pap smears and mammograms, resulting in women veterans being 46% more likely to receive community care than their male counterparts. This has led to women being disproportionately affected by billing problems, longer wait times and staffing shortages.
“For women, 30% of care is received in the community,” Hayes told subcommittee members. “That’s for maternity care, infertility care, and in some places mammograms. Also part of that is in-home care. As women age and live longer than men, they have more of the community care dollar. What’s most critical about community care is care navigation and care coordination.”
Currently, VA only has 65 sites with mammogram services, and they do not always correspond to where there are large concentrations of women veterans. Asked how VA determines where mammogram facilities are placed, Hayes explained that the two biggest barriers were personnel and physical space—factors that could be applicable to any number of types of healthcare.
“In most places, we do not have a significant enough population to be able to have the highest quality of mammogram. That’s critical to me. We don’t want women to be seen by someone who hasn’t seen enough mammograms,” Hayes explained. “One of the other big issues is space. It takes considerable space and lead-lined walls. We’re continuing to work with sites to see how they can prioritize adding radiology space and mammogram space.”
With many women veterans needing to fall back on receiving mammograms from community providers, VA is putting resources into making sure its properly coordinating that care.
“If we don’t have someone tracking to make sure that mammogram result gets noticed by the primary care providers, that it gets to the breast cancer surgeons, we’re in trouble,” Hayes said. “That’s the biggest part of what we’re doing. We’ve invested in mammogram coordinators and maternity care coordinators.”
VA’s goal is to have a designated women’s health provider at every facility, including its community-based outpatient clinics. With staffing shortages impacting healthcare facilities across the country, VA has sent training teams to facilities that aren’t able to hire new staff in order to train up existing staff on women’s healthcare needs.
“We’ve taken someone who is a good VA provider and really expanded their role to truly be a good provider for women veterans,” Hayes said.
“The obvious [improvements] include when you have a patient not having to go somewhere else for a Pap smear, because someone has been trained up using live models and is comfortable handling a Pap smear or a vaginal infection,” Hayes explained.
The more subtle improvements might be longer-lasting, since they focus on an understanding of the experience of women veterans in the military.
“These providers are trying on the battle rattle and realizing this complaint of musculoskeletal pain or headache or neck problem or joint problem is because of what that women had to do with all that equipment on,” Hayes said. “We’re also training them up a lot on military sexual trauma, interpersonal violence, depression and management of basic mental health conditions in the primary care setting.”
This effort to increase VA’s capacity to serve its women veterans might not be able to keep up with the growing influx of women into VA facilities, Hayes said. “We have such a wave of women coming in that, even with all the training we’re doing [it might not be enough]. This year we’re going to hit 700 providers trained, and we’ll still probably have a gap of 500-700 providers. We have an uphill battle here.”
1 Klap R, Darling JE, Hamilton AB, Rose DE, Dyer K, Canelo I, Haskell S, Yano EM. Prevalence of Stranger Harassment of Women Veterans at Veterans Affairs Medical Centers and Impacts on Delayed and Missed Care. Womens Health Issues. 2019 Mar-Apr;29(2):107-115. doi: 10.1016/j.whi.2018.12.002. Epub 2019 Jan 25. PubMed PMID: 30686577.

