
Michael Matheny, MD, MS, MPH, Associate Director of Health Services Research and Development, VA Informatics and Computing Infrastructure (VINCI)
NASHVILLE, TN — Fluoroquinolones (FQs) have long been a standard treatment for urinary tract infections (UTIs), offering effective relief for millions of patients worldwide.
Some studies have suggested, however, that the drugs might increase the risk of aortic aneurysm or dissection, leading to safety warnings and restrictions in certain patient population. Other studies have failed to show a connection.
Now, new research, using a more rigorous, large-scale approach, provides a clearer picture: Fluoroquinolones do not appear to elevate this risk when compared to other commonly used antibiotics.
The study, published in eClinicalMedicine after an extensive review of patient data, was conducted across five countries— the United States, South Korea, Japan, Taiwan and Australia. Researchers analyzed health records from 14 medical databases between 2010 and 2019, including data from over 13 million adults age 35 and older who were prescribed fluoroquinolones or alternative antibiotics like trimethoprim (with or without sulfamethoxazole) and cephalosporins. The study focused specifically on outpatient cases of UTIs, excluding patients recently hospitalized to ensure the findings applied to typical outpatient antibiotic use.1
The concern about fluoroquinolones stems from the possibility that they may weaken connective tissues by increasing the activity of enzymes that break down collagen, a key protein in blood vessels, said Michael Matheny, MD, MS, MPH, associate director of Health Services Research and Development, VA Informatics and Computing Infrastructure (VINCI), who is one of the study’s authors. “This could, in theory, make the aorta more vulnerable to aneurysms or dissections However, the evidence for this mechanism in humans has been inconsistent.”
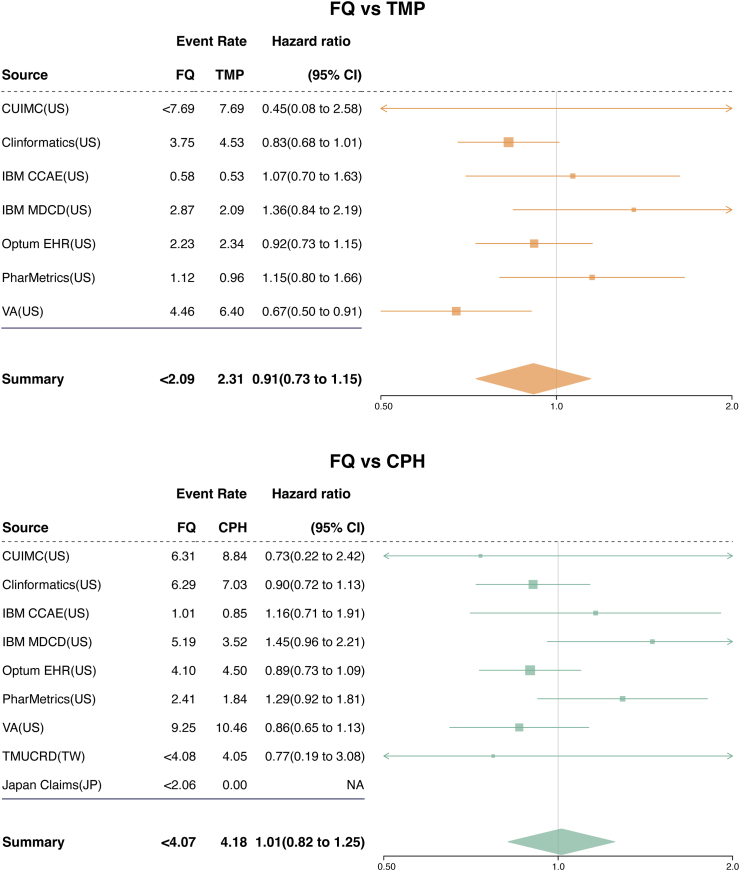
Click to Enlarge: Meta-analytic comparative risk of aortic aneurysm or dissection within 60 days after treatment initiation for urinary tract infection. The forest plots show the calibrated hazard ratios (HRs) and 95% confidence intervals (CIs) for the risk of aortic aneurysm or dissection within 60 days after treatment initiation with fluoroquinolones (FQs) compared to trimethoprim with or without sulfamethoxazole (TMP) or cephalosporins (CPHs) for urinary tract infection. The event rates per 1000 person-years for each treatment group are also provided. In databases where the number of outcome events was less than 5, the exact count was not collected to protect patient privacy. The HRs were estimated using Cox proportional hazards models after propensity score matching in each database. The HRs were then calibrated based on the empirical null distribution derived from negative control outcomes to account for systematic bias. The calibrated HRs from each database were pooled using a Bayesian random-effects meta-analysis with non-normal likelihood approximations. The size of the data marker indicates the weight of the study. Error bars indicate 95% CIs. Abbreviations: FQ, fluoroquinolone; TMP, trimethoprim with or without sulfamethoxazole; CPH, cephalosporin; CI, confidence interval; CUIMC, Columbia University Irving Medical Center data warehouse; Clinformatics, Optum’s Clinformatics® Data Mart Database; IBM CCAE, IBM Health MarketScan® Commercial Claims and Encounters Database; IBM MDCD, IBM Health MarketScan® Multi-State Medicaid Database; Optum® EHR, Optum© de-identified Electronic Health Record Dataset; PharMetrics, PharMetrics Plus; VA, Department of Veterans Affairs; TMUCRD, Taipei Medical University Clinical Research Database; NA, not applicable. Source: eClinicalMedicine
Designed to address previous limitations, the study applied advanced statistical techniques to minimize bias and confounding factors. To ensure a fair comparison between groups, the researchers employed a method called propensity score-matching. This statistical tool helps balance variables like age, existing health conditions and other potential confounders between the fluoroquinolone group and those receiving alternative antibiotics. After refining the data, the researchers ended up with about 3.9 million patients in the fluoroquinolone-TMP comparison and about 2.4 million in the fluoroquinolone-cephalosporin comparison, Matheny told U.S. Medicine.
No Difference Among Antibiotics
The findings: There was no real difference in the risk of aortic aneurysm or aortic dissection between people who took fluoroquinolones and those who took other antibiotics. The researchers measured the risk using a statistic called a hazard ratio, which showed that fluoroquinolones were no more likely to cause these conditions than the other antibiotics. For example, compared to TMP, the risk was 0.91, and compared to cephalosporins, it was 1.01 — both of which mean there was no increased danger. Since earlier studies raised concerns that fluoroquinolones might be harmful to the aorta, these results suggest that those concerns were likely overstated.
One major strength of the study, which was funded in part by VINCI, lies in its breadth and methodology. “Many earlier studies had limitations, such as not using active comparator antibiotics, failing to control for underlying health conditions or relying on smaller, localized datasets,” Matheny explained. “Some may have misattributed the risk of aortic complications to fluoroquinolones, when the real risk factor was the underlying infection or the patient’s existing health conditions. Our study used a larger, more diverse dataset and more advanced statistical methods to reduce bias, which may explain why our results differ from some prior studies.”
He pointed out that the findings suggest that concerns about aortic aneurysm or dissection should not be a deciding factor when prescribing fluoroquinolones for urinary tract infections in an outpatient setting. “While fluoroquinolones should still be used carefully—due to risks like antibiotic resistance and other potential side effects — our results do not support restricting their use solely due to concerns about AA/AD risk.”
As with all drugs, clinicians should continue to weigh overall risks and benefits when prescribing antibiotics, considering factors like antibiotic resistance, patient history and alternative treatment options, Matheny noted. “However, concerns about AA/AD should not be a primary reason to avoid fluoroquinolone use in otherwise appropriate cases.”
- Janetzki JL, Kim JH, Minty E, Lee JA, et al. Risk of aortic aneurysm or dissection following use of fluoroquinolones: a retrospective multinational network cohort study. EClinicalMedicine. 2025 Feb 1;81:103096. doi: 10.1016/j.eclinm.2025.103096. PMID: 39975698; PMCID: PMC11836508.

