PROVIDENCE, RI — Servicemembers with prolonged deployment to military bases with open burn pits might have an increased risk for developing adverse health conditions, such as respiratory and cardiovascular disease, according to a recent study.
The retrospective observational cohort study, led by researchers from the Providence, RI, VAMC, was published in JAMA Network Open.1
Many veterans who served in Afghanistan during Operation Enduring Freedom (2001-2014) and Iraq during Operation Iraqi Freedom (2003-2011) were deployed to military bases with open burn pits and exposed to their emissions, according to the report. The U.S. military used open burn pits on some military bases to dispose of solid, medical and hazardous materials. In 2009, the DoD restricted materials allowed in burn pits and continued to use them until other methods (e.g., incineration, recycling, waste segregation, landfill) were implemented. There is limited understanding of the long-term health consequences of this exposure, the study authors pointed out.
This study involved 459,381 military veterans from Operation Enduring Freedom and Operation Iraqi Freedom who received healthcare from the VHA. The authors used VHA medical records and declassified deployment records from the DoD to assess Army and Air Force veterans who were deployed between 2001 and 2011 and received healthcare afterward from the VHA, with follow-up through December 2020. Data were analyzed from January 2023 through February 2024, the authors said.
The study population, which was predominantly male (87%), had a mean age of 31.6 years. The population was racially and ethnically diverse, with 75,258 Black veterans (16.4%), 52,527 Hispanic veterans (11.4%) and 305,996 white veterans (66.6%). There was extensive variability in socioeconomic status indicators, and nearly half had smoked cigarettes at least some of the time, according to the study.
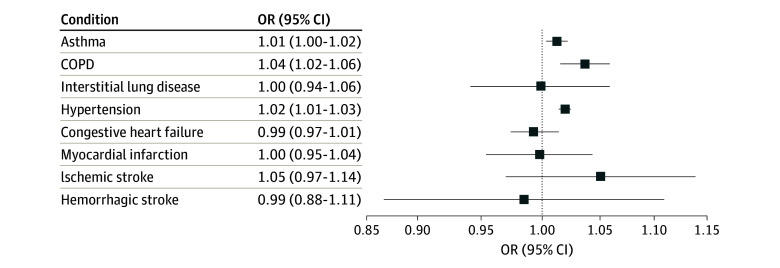
Click to Enlarge: Associations of Open Burn Pit Exposure With Respiratory and Cardiovascular Disease Outcomes in a Cohort of US Military Veterans (N = 459 381)
All odds ratios (ORs) are adjusted for age at Veterans Health Administration enrollment, sex (male or female), race and ethnicity (Black or not Black), region (Northeast, Midwest, South, West), median income of Census tract, percentage with a bachelor’s degree in census tract, body mass index (calculated as weight in kilograms divided by height in meters squared; >30 or ≤30), cigarette smoking (never, always, or mixed), Veterans Health Administration enrollment priority (service connected or disability, low income, low priority or high copay), branch of service (Army or Air Force), rank (officer, enlisted, or unknown), year of entry for Veterans Health Administration care, deployment duration, square of deployment duration, and cube of deployment duration. Source: JAMA Network Open
The authors reported that most of the cohort had been assigned to bases with burn pits at some point (392,865 veterans, or 85.6%). The overall median exposure was 244 days, and the median duration of deployment to bases with burn pits within the tertiles was 129 days in the lowest exposure group, 272 days in the middle exposure group and 474 days in the highest exposure group. More than half of those with no documented exposure to burn pits were deployed to countries other than Afghanistan or Iraq (e.g., transit bases mostly in the region), which was 35,890 veterans or 54.0%.
The median duration of deployment was 353 days for the full cohort, with medians of 290 days for the no-exposure group, 281 days for the lowest exposure group, 342 days for the middle exposure group and 651 days for the highest exposure group. Median follow-up from end of deployment was 10.9 years. The analysis measured odds of diagnosis of asthma, chronic obstructive pulmonary disease, interstitial lung disease, hypertension, myocardial infarction, congestive heart failure, ischemic stroke and hemorrhagic stroke, the researchers pointed out.
“We found evidence of a small increase in risk of asthma, chronic obstructive pulmonary disease, hypertension and ischemic stroke with longer periods of deployment to bases with burn pits,” Amal N. Trivedi, MD, MPH, of the Providence VAMC and Brown University School of Public Health, told U.S. Medicine.
Continuous Exposure
For every 100 days of deployment to bases with burn pits, “veterans experienced increased adjusted odds for asthma, chronic obstructive pulmonary disease, hypertension and ischemic stroke. Odds of interstitial lung disease, myocardial infarction, congestive heart failure or hemorrhagic stroke were not increased. The results based on tertiles of duration of burn pit exposures were consistent with those from the continuous exposure measures,” according to the authors.
The study noted that, “while the associations were modest in magnitude, there are several million potentially affected veterans, making any elevation in risk important to document.”
“Heightened awareness of the history of exposure to open burn pits and careful assessment of chronic respiratory and cardiovascular disease continue to be a high priority for patients and their care providers,” Trivedi explained. “The questions regarding long-term health consequences of exposure to open burn pits remain a concern, and this study provides some evidence that certain chronic diseases may be related to that exposure. Given the PACT Act, this study offers some new information regarding hazardous exposures associated with deployment to Afghanistan and Iraq.”
While the associations are of some concern given the large numbers of individuals who served in Operation Enduring Freedom and Operation Iraqi Freedom, the small magnitude of increases identified would not change recommendations regarding health care of veterans, Trivedi advised.
An important result of this study is “the successful linkage of data from DoD on deployment history to long-term health outcomes among those receiving care through the VA,” he pointed out, adding, “This linkage should be valuable in addressing a wide range of potential health hazards associated with military service.”
Previous studies have “attempted to directly examine the association between burn pit exposures and health outcomes, but this study provides new information on the long-term health outcomes associated with burn pit exposures due to strengths that distinguish it from previous analyses. These strengths include a much larger population, individual-level reconstruction of each veteran’s history of deployment to bases with burn pits using declassified military records, and a long follow-up time for assessment of health outcomes,” study authors suggested.
In addition, using “VHA health care records to identify clinical diagnoses over the entire period after initial enrollment minimized loss to follow-up or dependence on self-reported health conditions,” according to the report.
- Savitz DA, Woskie SR, Bello A, Gaither R, Gasper J, Jiang L, Rennix C, Wellenius GA, Trivedi AN. Deployment to Military Bases With Open Burn Pits and Respiratory and Cardiovascular Disease. JAMA Netw Open. 2024 Apr 1;7(4):e247629. doi: 10.1001/jamanetworkopen.2024.7629. PMID: 38662371; PMCID: PMC11046344.


