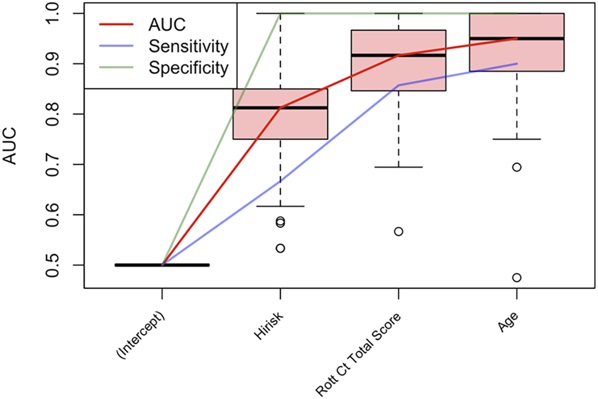
Click to Enlarge: Ranked predictors of post-traumatic vasospasm after severe traumatic brain injury using LASSO, 100-fold cross-validation. The pink box plots show the range of AUC scores encountered during cross-validation. The addition of triple risk from the CART analysis, Rotterdam computed tomography total score, and age progressively improved model accuracy. AUC, area under curve. Source: CNS Neuroscience
BETHESDA, MD — Serum cytokines, neuronal proteins and clinical data can be used to predict vasospasm and early mortality in patients with severe traumatic brain injury, according to a recent study.
The study published in the journal Neurosurgery was designed to identify early clinical characteristics, serum inflammatory cytokines and neuronal-specific proteins that may be used as biomarkers alone or in combination to predict post-traumatic vasospasm in civilian patients with severe traumatic brain injury. The authors also aimed to improve the prediction of patient outcomes after severe traumatic brain injury, which is limited with current clinical tools, by using these variables to develop predictive models for post-traumatic vasospasm and mortality.1
The study was led by researchers from Sierra Neurosurgery Group in Reno, NV, and
Emory University in Atlanta and included participation from the Uniformed Services University of the Health Sciences, Walter Reed National Military Medical Center and the Henry M. Jackson Foundation for the Advancement of Military Medicine Inc., all in Bethesda, MD.
Post-traumatic vasospasm, a potential complication of primary head injury, can lead to secondary injury and possibly worse neurologic recovery. Past research has found that post-traumatic vasospasm is common, occurring in 35% to 48% of civilian traumatic brain injuries with rates as high as 71% after severe injury, according to the researchers.
Vasospasm is challenging to diagnose in severely injured patients, and transcranial Doppler might not be possible. As a result, rapid-screening tools could help clinicians, particularly in resource-poor or active combat settings, to identify patients at highest risk of post-traumatic vasospasm, provide closer monitoring and detect patients at risk of early death from severe traumatic brain injury. Rapid screening tools could also provide information on serum inflammatory or neuronal markers associated with developing post-traumatic vasospasm, the authors pointed out.
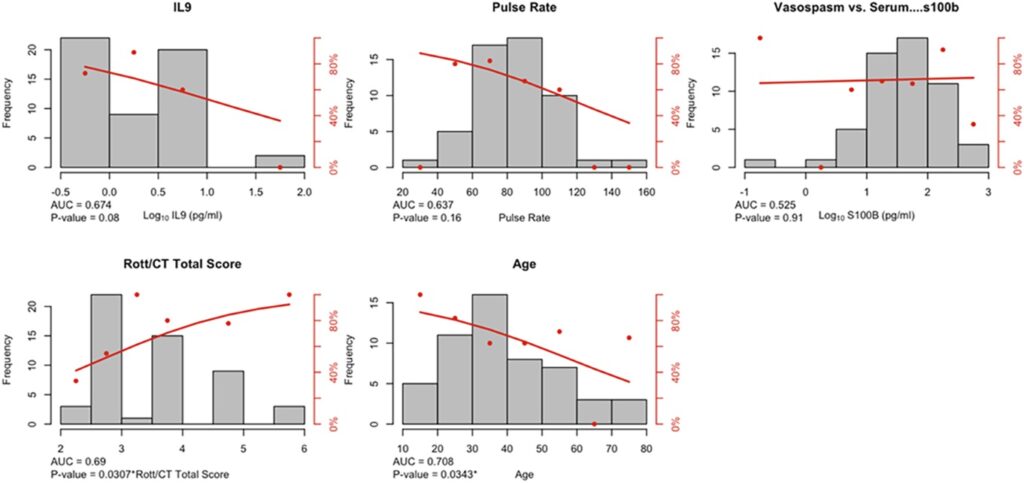
Click to Enlarge: Univariate comparisons of predictor variables for patients with post-traumatic vasospasm. The gray bars represent the distribution of the predictor variable, while the red dots and regression line represent the risk of vasospasm. Three of 5 predictors fail to achieve statistical significance on a univariate basis, but are significant after adjusting for other predictors. AUC, area under curve; CT, computed tomography. Source: CNS Neuroscience
This study included 53 adult civilian patients enrolled in the severe traumatic brain injury arm of the Surgical Critical Care Initiative, a consortium of federal and nonfederal research institutions focused on delivering precision medicine to individual patients by developing, translating and validating biology-driven critical care. Study participants were adults (18 years and older) who presented to Grady Memorial Hospital in Atlanta with severe traumatic brain injury and abnormal neuroimaging findings. Excluded were patients who had isolated diffuse axonal injury, bilateral fixed and dilated pupils, incarceration or pregnant status, the researchers explained.
The investigators collected clinical data by chart review, including injury timeline, mechanism, characteristics, admission Glasgow Coma Scale and pupillary response, and they combined clinical, serum inflammatory and neuronal protein data to construct models for predicting development of post-traumatic vasospasm and mortality. Patients were evaluated every 6 hours, as available, for the following variables: vital signs, complete blood count, basic metabolic panel, coagulation studies, arterial or venous blood gas values, urinalysis and urine toxicology. The patient’s admission head computed tomography imaging also was evaluated.
Serum samples were collected within 72 hours of admission and analyzed for an array of inflammatory and neuronal-specific markers. After informed consent, serum was obtained daily for 14 days, every other day for 14 days, then weekly until discharge. In addition, patients were screened for post-traumatic cerebral vasospasm for the first seven days after injury following enrollment, or longer as clinically indicated.
Vasospasm was categorized as mild, moderate or severe. Severe vasospasm was confirmed with CT angiogram and treated. The authors also documented inpatient mortality and assessed long-term survival and functional outcome via written questionnaires and phone interviews, according to the study.
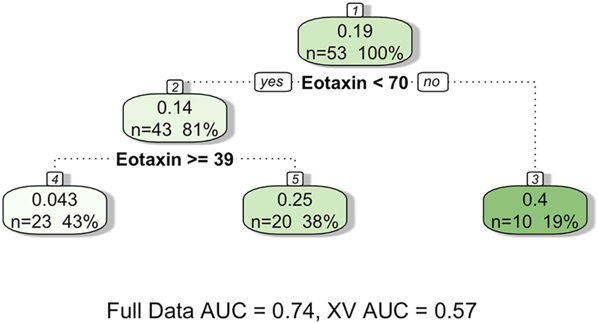
Click to Enlarge: Risk factors for mortality after severe traumatic brain injury using CART. Only 2 rules were needed to identify a low-risk category (43% of patients, 4.3% mortality risk) and a high-risk category (19% of patients, 40% mortality risk). AUC, area under curve; CART, classification and regression trees. Source: CNS Neuroscience
Study authors concluded that inflammatory cytokine levels after severe traumatic brain injury might have predictive value that exceeds conventional clinical variables for certain outcomes. They identified several factors that are beneficial in predicting development of post-traumatic vasospasm, including IL-9, pulse rate and eotaxin, as well as Rotterdam CT Score of Traumatic Brain Injury and age. The researchers also determined that eotaxin, IL-6, IL-12 and glucose were predictive of mortality. IL-6, IL-9 and IL-12 are proinflammatory cytokines, and eotaxins are small proteins.
Among the 53 participants, the study found that 36 (67.9%) patients developed vasospasm and 10 patients (18.9%) died. Many developed moderate to severe vasospasm (42%), with three patients requiring treatment (8.3%). Most injuries resulted from falls (n = 10, 18.9%) or motor vehicle collisions (n = 32, 60.4%). The mean age of participants was 39.2 years old, and 12 patients (22.6%) were women.
The predictive model called classification and regression trees (CART) identified lower IL-9, lower presentation pulse rate and higher eotaxin as predictors of vasospasm development. The data analysis method known as least absolute shrinkage and selection operator (LASSO) identified higher Rotterdam computed tomography score and lower age as risk factors for vasospasm development, according to the researchers.
The investigators also found that CART identified high levels of eotaxin as most predictive of mortality, while LASSO identified higher serum IL-6, lower IL-12 and higher glucose as predictive of mortality.
Limitations of this study include its exploratory nature, small cohort size and omission of serum sampling and vasospasm screening in the early days after injury for some patients. This study’s predictive model for post-traumatic vasospasm could be used to identify patients at highest risk of death for early triage and serve as a resource in resource-poor or combat settings, the investigators explained.
- Rindler RS, Robertson H, De Yampert L, Khatri V, Texakalidis P, Eshraghi S, Grey S, Schobel S, Elster EA, Boulis N, Grossberg JA. Predicting Vasospasm and Early Mortality in Severe Traumatic Brain Injury: A Model Using Serum Cytokines, Neuronal Proteins, and Clinical Data. Neurosurgery. 2024 Oct 11. doi: 10.1227/neu.0000000000003224. Epub ahead of print. PMID: 39471078.

