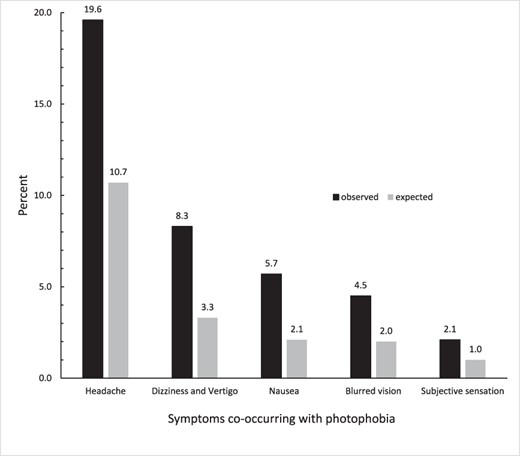
Click to Enlarge: Comparison of percentages of observed versus expected co-occurrences for 5 symptoms with photophobia at the encounter level. Co-occurrence comparisons were positively associated for each symptom (P < .00001).
Source: AMSUS: Military Medicine
FALLS CHURCH, VA — After a mild traumatic brain injury (mTBI), military servicemembers who suffer from photophobia, a symptom of visual discomfort in response to normal light levels, often show a decline in photophobia within 30 days of the injury, according to a recent study.
The study, published in Military Medicine, characterized comorbid conditions and symptoms in mTBI patients with photophobia to assess their co-occurrence, describe the persistence of photophobia and assess the effectiveness of using currently available codes in reporting photophobia.1
The study authors are affiliated with the Defense Health Agency in Falls Church, VA, and Walter Reed National Military Medical Center in Bethesda, MD.
“Individuals who sustain concussion and/or traumatic brain injury frequently experience heightened sensitivity to light, or photophobia,” Natalya Merezhinskaya, PhD, a health science specialist in the Vision Center of Excellence at the Defense Health Agency, Research and Engineering Directorate, told U.S. Medicine. “This symptom can significantly affect readiness, performance and activities of daily living of servicemembers and veterans.”
Photophobia is “one of the most common complaints following mild traumatic brain injury,” the authors reported. “Studies have found that 50% of active-duty war fighters and 55% of veterans were diagnosed with photophobia following mild traumatic brain injury. This abnormal intolerance to light can adversely affect critical aspects of functioning, including information processing, communication, cognition, sleep and mental health.”
Although photophobia is a frequent complaint, “diagnosis is mostly based on self-reports or questionnaires because of the lack of objective validated tools, and analyses are limited, since photophobia doesn’t have a specifically dedicated International Classification of Diseases (ICD) code that makes it easily identifiable when data mining electronic health records,” the researchers explained.
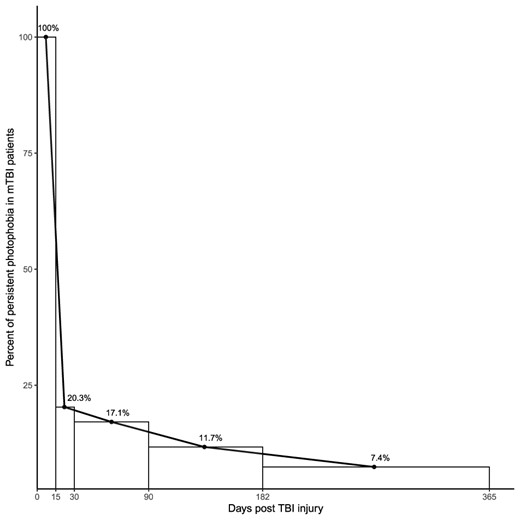
Click to Enlarge: Percent persistence of photophobia symptom in mTBI cohort within 365 days after the injury. The numbers were summarized for the intervals of 0-15, 16-30, 31-90, 91-183, and 184–365 days. Vertical lines indicate the reported time intervals.
Source: AMSUS: Military Medicine
“We wanted to look at how long photophobia persists after the head injury, since this is an important factor for the healthcare providers to consider while managing patients with mild traumatic brain injury (TBI),” Merezhinskaya said. “We also wanted to see whether there are other symptoms that are frequently observed together with the sensitivity to light. This may give clinicians some clues about the common mechanism(s) of photophobia and comorbid conditions and facilitate development of successful treatments based on the common underlying deficits.”
Using the defense and veterans eye injury and vision registry, the authors identified 639 servicemembers diagnosed with photophobia after mTBI (based on the Armed Forces Health Surveillance Board criteria). Photophobia and other potentially related conditions and symptoms were obtained from the medical records. To ensure the photophobia was associated with head injury, only servicemembers who had their first indication of photophobia within 15 days after the injury and with no complaint of photophobia for a year before the injury were included. Servicemembers with concomitant eye injury that could elicit photophobia were excluded from the study, according to the authors.
The research team analyzed the co-occurrence of photophobia with these conditions or symptoms, assessed the persistence of photophobia up to one year after the injury and evaluated the utilization of currently available ICD codes for photophobia, the study reported.
“We found that servicemembers who experienced mild TBI and who had light sensitivity, or photophobia, after the head injury, also very often had headaches, dizziness and nausea,” Merezhinskaya said. “In the majority of these servicemembers, light sensitivity subsided within 30 days after the injury; however, some individuals continue experiencing photophobia up to a year after TBI.”
The study’s results indicate a strong relationship between photophobia and headache after a mild traumatic brain injury. The analysis determined that “92% of the servicemembers with photophobia after mild traumatic brain injury also experienced headaches. Dizziness/vertigo and nausea were also frequent complaints in this group,” she pointed out.
“The connection between the light sensitivity and headaches has been described for other populations of individuals after concussion,” according to Merezhinskaya. “Our findings indicate that additional research is needed to better understand this relationship. It is important for the healthcare providers to take a detailed medical history of a patient post-TBI to record all pertinent symptoms. It is especially pertinent to photophobia since this symptom does not have a dedicated International Classification of Diseases (ICD) code, which makes it more difficult to uniformly report.”
Healthcare professionals who are treating servicemembers and veterans after traumatic brain injury “need to take a detailed medical history that includes questions about light sensitivity and comorbid conditions in order to understand the full scope of the impact of the injury and their possible interconnectedness,” she explained.
“We suggested that the medical community might consider introducing a dedicated ICD code for photophobia in the future,” Merezhinskaya added. “For the majority of the servicemembers, light sensitivity diminished within the 30 days since the injury. However, for some individuals, photophobia persisted for up to a year. It will be important to look specifically at chronic light sensitivity to determine what factors might determine higher susceptibility to this condition.”
A dedicated ICD code for photophobia “will help to record, report and analyze the data much more extensively,” she advised.
- Merezhinskaya N, Bai AC, Park D, Barker Ii FM, Gu W. Characterization of Mild Traumatic Brain Injury Cohort With Photophobia From the Defense and Veterans Eye Injury and Vision Registry. Mil Med. 2024 Aug 19;189(Supplement_3):736-742. doi: 10.1093/milmed/usae251. PMID: 39160895.
