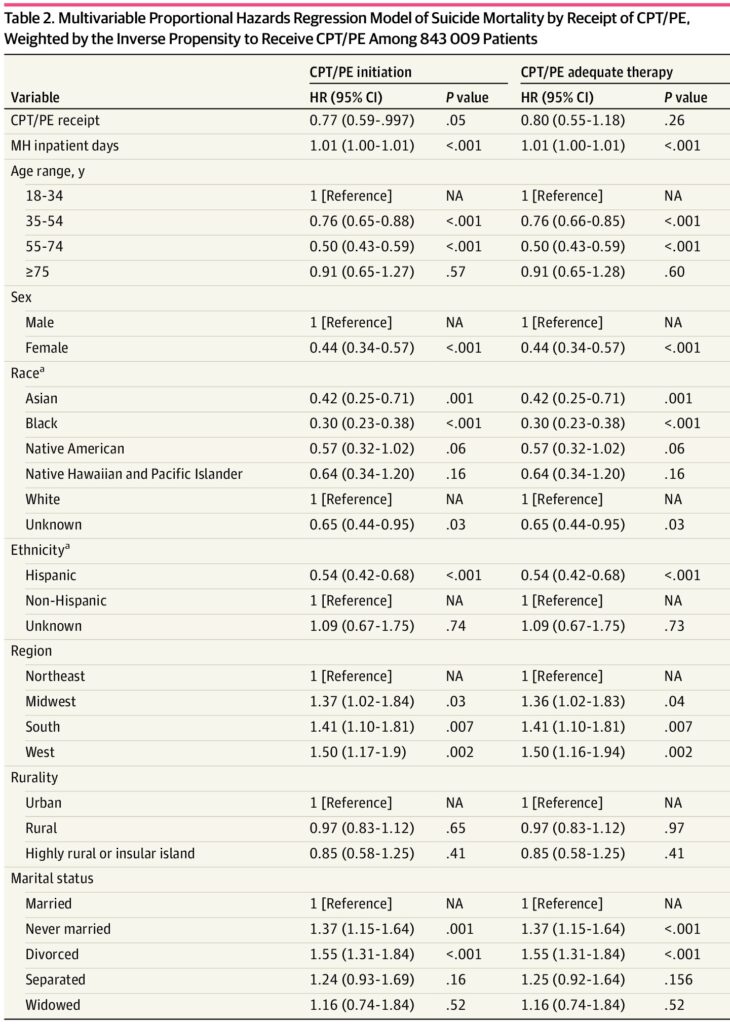
Click to Enlarge: Multivariable Proportional Hazards Regression Model of Suicide Mortality by Receipt of CPT/PE, Weighted by the Inverse Propensity to Receive CPT/PE Among 843 009 Patients Abbreviations: CPT, cognitive processing therapy; HR, hazard ratio; MH, mental health; NA, not applicable; PE, prolonged exposure.
a. Data on race and ethnicity were extracted from the US Veterans Affairs Corporate Data Warehouse. No further breakdown of the classifications is available. Source: JAMA Network Open
ANN ARBOR, MI — Suicide prevention is the top clinical priority of the VA. Given the higher prevalence of PTSD among veterans and its strong association with veteran suicide risk, it is essential to evaluate whether and how the treatments veterans receive for PTSD through the VA are influencing that risk.
A recent study highlighted the impact of two first-line treatments recommended for PTSD—cognitive processing therapy (CPT) and prolonged exposure (PE). It also raises concerns that only a small percentage of veterans who could benefit from these therapies have received them.
CPT is a type of cognitive behavioral therapy that helps individuals reduce the emotional impact of trauma by identifying and challenging unhelpful beliefs through structured discussions, written trauma narratives and cognitive exercises. PE aims to reduce PTSD symptoms by having individuals repeatedly recount their trauma and gradually face avoided situations in a safe, controlled manner to desensitize fear responses.
“CPT and PE had already been shown to reduce suicidal ideation among veterans, but there had not been any large-scale studies of suicide risks associated with receiving CPT or PE,” said Kevin Saulnier, PhD, a research investigator at the Center for Clinical Management Research, VA Ann Arbor, MI, Healthcare System and first author of the new study.
To support VHA clinically based suicide prevention activities and enhance clinical operations, Saulnier and his VA colleagues examined suicide risk among veteran patients after they were initially diagnosed with PTSD. “We identified CPT and PE sessions via standard note templates stored in VA’s electronic medical record,” Saulnier said. “These note templates are used when providers document CPT and PE visits.” 1
The study, published in JAMA Network Open, looked at both initiation and adequacy of CPT/PE therapy. Adequate CPT/PE therapy was defined as the receipt of 8 or more sessions of CPT or PE within a 180-day period because these treatments are designed to be delivered in a time-limited fashion, with a full course of CPT/PE generally requiring 8 to 9 sessions, and many patients reporting clinically significant improvements within 8 sessions, the authors stated.
“Recognizing this time course, many studies of psychotherapy adequacy use 8 sessions as a metric for minimally adequate therapy, and 8 sessions is used as a mental health performance measure in VHA.”
Suicide deaths were identified using death records.
Of the population-based sample of 847,217 U.S. veterans, most were male (86.9%), and the mean age was 50.1 years. From the initial PTSD diagnosis (during 2016-2019) through 2020, there were 1,552 suicides. A total of 73,473 individuals (8.7%) initiated CPT/PE, with 33, 931 of those patients (46.2% of those with any CPT/PE) attending 8 or more sessions and being classified as having received an adequate course of therapy. Of the cohort, 1,552 individuals (0.2%) died by suicide during the follow-up period.
Multivariable proportional hazards regression indicated that initiation of CPT/PE treatment was associated with a 23% lower suicide risk compared with those who did not initiate CPT/PE; however, receipt of an adequate course of treatment was not significantly associated with suicide.
Although 65.2% of the cohort received psychotherapy, concerningly “only 8.7% of veteran VHA patients with newly diagnosed PTSD received CPT or PE,” Saulnier said. “This suggests that continued efforts are needed to increase the availability of evidence-based PTSD interventions for veterans with this condition.”
“These findings, and previous work, suggest that the investments VA has made in expanding access to evidence-based PTSD treatments have paid off for both treating PTSD and also as a critical component of suicide prevention efforts,” Saulnier told U.S. Medicine. “For providers, these findings give helpful context regarding PTSD treatment in the setting of suicide risk.”
“Some providers may choose to wait until suicide risk subsides before starting an evidence-based treatment for PTSD due to concerns about readiness to engage in trauma work,” he continued. “Our findings suggest that those concerns may be overblown and that initiating CPT or PE may be helpful for both treating PTSD and also preventing suicide in this population.”
- Saulnier KG, Brabbs S, Szymanski BR, Harpaz-Rotem I, McCarthy JF, Sripada RK. Suicide Risk Among Veterans Who Receive Evidence-Based Therapy for Posttraumatic Stress Disorder. JAMA Netw Open. 2024 Dec 2;7(12):e2452144. doi: 10.1001/jamanetworkopen.2024.52144. PMID: 39724372; PMCID: PMC11672158.


