Study Linked Severe Sleep Problems with PTSD, Suicide

A soldier sleeps in a hasty fighting position on a cold morning in the mountains near Sar Howza, Paktika province, Afghanistan, in 2009. Army photo by Staff Sgt. Andrew Smith
SAN DIEGO—Recent veterans who receive care at the VA have “alarmingly high” rates of insomnia disorder, according to a new study finding that the condition was diagnosed in more than half of the sample studied.
The article in the Sleep journal noted that post-9/11 veterans are especially susceptible to insomnia disorder. “Having accurate prevalence rates of insomnia disorder in this relatively young, diverse population is vital to determine the resources needed to identify and treat insomnia disorder,” wrote the VA San Diego Healthcare System-led researchers.
To remedy that, the study team sought to create a documented prevalence rate of insomnia disorder, and correlates in a large sample of post-9/11 veterans who were VHA beneficiaries.
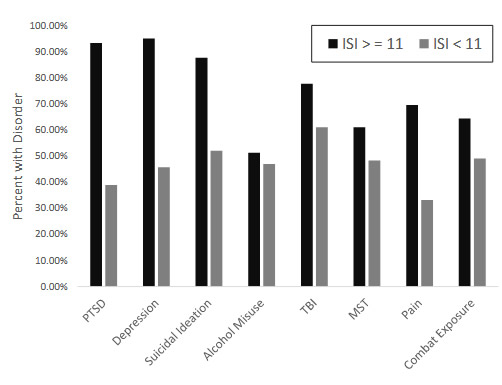
Their observational study focused on 5,552 post-9/11 veterans newly enrolling for healthcare. Researchers collected data using VA eScreening. Participants were assumed to have an insomnia with a clinical cutoff score of greater than or equal to 11 on the Insomnia Severity Index (ISI). Also included in the analysis were sociodemographic information, service history, posttraumatic stress disorder (PTSD), depression, suicidal ideation, alcohol misuse, military sexual trauma (MST), traumatic brain injury (TBI) and pain intensity.
Results indicated that 57.2% of the sample population had insomnia disorder. “Our sample was nationally representative for age, sex, ethnicity, branch of the military, and race,” the authors explained. “The
sample also was at high-risk for a host of clinical disorders, including PTSD, TBI, and pain; all of which showed higher rates of insomnia disorder (93.3%, 77.7%, and 69.6% respectively).”
The authors emphasized, “Rates of insomnia disorder in post-9/11 veterans is alarmingly high and requires increased attention and direct treatment, especially in the context of co-occurring disorders.”
Background information in the article pointed out that veterans are particularly vulnerable to insomnia and often have rates two-to-three times that of civilian populations. One reason, the authors suggested, is that sleep/wake schedules during active duty are so irregular. They also have faced harsh living conditions, combat stress and higher rates of physical and psychological injury during deployment. Those veterans also sometimes struggle with post-deployment reintegration, according to the report.
“Insomnia disorder among Veterans Health Administration (VHA) users is expected to continue rising as post-9/11 troops leave military service and begin accessing VHA healthcare,” the researchers cautioned.
The authors, who also were from Duke University School of Medicine and the Durham, NC, Center of Innovation to Accelerate Discovery and Practice Transformation, explained why their estimates of insomnia disorder in recent veterans are so much higher than previous studies. They noted that several studies have reported prevalence rates of insomnia symptoms using “trouble falling or staying sleep” assessed from other military health questionnaire, finding rates of insomnia symptoms of 24.7%-0.5% in a general military/veteran population to upward of 100% in Vietnam veterans with PTSD.
“However, a single item about sleep is not a validated measure of insomnia diagnosis, may be anchored to other items in the questionnaire, and may be overly influenced by external factors,” the researchers advised.
They also questioned the results of reviews using ICD-9 diagnostic codes from large national VHA databases to estimate prevalence rates of insomnia disorder. Those studies determined that 2.5% of 9,786,778 U.S. veterans seeking VA healthcare from 2000 to 2010 had an insomnia diagnosis recorded in their medical record, with the one-year (2010) prevalence rate of insomnia diagnosis at.4% in veterans.2,3
While those studies indicated that PTSD was associated with the highest prevalence of insomnia (16%) and linked deployments to Iraq or Afghanistan conflicts, anxiety and depressive disorders to insomnia, the authors commented, “Unfortunately, using medical records does not provide accurate prevalence of insomnia disorder. Only 53% of VA primary care providers indicated routinely documenting insomnia disorder and 39% routinely included it in the problem list.”
They argued that, with community insomnia rates of 6%-10%, “the rates suggested by these large studies severely underrepresent the true prevalence of insomnia disorder in veterans.”
The study warned that insomnia is predictive of the development and recurrence of mood disorders and suicidality, while being associated with the severity of psychiatric conditions, such as PTSD. “Collectively, insomnia disorder is a risk factor for the most common medical and MH conditions seen in veterans, yet, insomnia disorder often goes unscreened and untreated in the VHA,” it noted.
The authors pointed to the large discrepancy between actual prevalence rates of insomnia disorder and what providers are documenting, pointing out that, while medical record codes have found rates 2.5% and 3.4%, their study calculated the rate at 57.2% using an independent measure of insomnia. “This confirms and expands on the finding that fewer than half of VHA providers routinely include insomnia in the encounter problem list,” they explained, positing that physicians tend to focus on the “root cause” of insomnia—such as PTSD or pain—instead of looking at issues such as conditioned arousal. That could be preventing effective insomnia treatment, researchers suggested.
While certain factors—mental health disorders, increased combat exposure, positive for traumatic brain injury or military sexual trauma, higher pain—were all correlated with significantly higher rates of insomnia disorder, researchers said they were surprised that other issues were not. In fact, the study pointed out that neither the number of deployments nor screening positive for alcohol misuse seemed to have any effect on insomnia screening.
A troubling result, however, was that screening positive for suicidal ideation was strongly associated with insomnia disorder, the authors added, and “screening positive for PTSD and depression was associated with incredibly high rates of insomnia disorder.”
The authors suggested several explanations for their findings:
- The higher prevalence of insomnia reported here, as compared to previous research, might reflect high rates of combat exposure (53.7%) in their sample.
- The co-occurrence of high PTSD and depression might have an additive effect in insomnia prevalence.
- The cutoff of the insomnia measure of greater than or equal to 11 might not have been high enough for a complex PTSD veteran sample and should have been greater or equal to 15.
“Our study suggests a critical need to increase evidence-based treatments for insomnia, especially in individuals with co-occurring disorders; this may be especially pertinent to help combat suicidal ideation in veterans,” the researchers wrote, noting that cognitive behavioral therapy for insomnia (CBT-I) is considered the front-line treatment for insomnia66 and is better than pharmacological interventions with longer lasting positive outcomes.
“Despite clear recommendations in the Department of Veterans Affairs/Department of Defense (VA/DOD) Clinical Practice guidelines, access to CBT-I as the standard of care for insomnia disorder is limited,” the study noted. “There is even increasing evidence in support of integrated treatment, providing CBT-I plus evidence-based treatment for the primary presenting disorder. Together examining and treating insomnia disorder in the context of co-occurring disorders, especially PTSD, depression, and suicidal ideation in the VHA system is a necessity.”
- Colvonen PJ, Almklov E, Tripp JC, Ulmer CS, Pittman J, Afari N. Prevalence Rates and Correlates of Insomnia Disorder in Post-9/11 Veterans Enrolling in VA Healthcare [published online ahead of print, 2020 Jun 12]. Sleep. 2020;zsaa119. doi:10.1093/sleep/zsaa119
- Alexander M, Ray MA, Hébert JR, et al. The national veteran sleep disorder study: Descriptive epidemiology and secular trends, 2000-2010-. 2016;39(7):1399-1410
- Hermes E, Rosenheck R. Prevalence, pharmacotherapy and clinical correlates of diagnosed insomnia among veterans health administration service users nationally. Sleep Med. 2014;15(5):508-514.

