More Screening Recommended
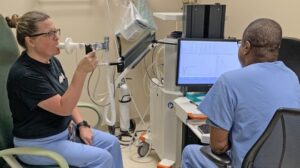
Many VA clinics offer TeleSpirometry, demonstrated in this photo, where lung function results are forwarded to a pulmonologist for review. New research has found a strong link between abnormal spirometry results and mental health issues. Photo from VA News. Nov 17, 2023
BOSTON — Veterans with obstructive respiratory disease should receive timely screening and treatment for comorbid psychiatric and medical conditions that frequently accompany the condition, according to a new study.
Researchers from the VA Boston and Connecticut healthcare systems as well as representatives from the Harvard and Yale schools of medicine sought to examine the psychiatric and physical health burden of obstructive respiratory disease in a nationally representative sample of U.S. veterans.
Key symptoms of the diseases—breathlessness, wheezing, cough and chest tightness—have been linked to high rates of emergency-room visits and hospitalization, but their impact goes well beyond their effects on the lungs, confirmed a new study examining both the physical and mental health burden associated with obstructive respiratory diseases in veterans.
Previous research has shown that obstructive respiratory diseases are highly comorbid with psychiatric and medical conditions. COPD, for example, is comorbid with other medical conditions, including heart failure, ischemic heart disease, lung cancer, diabetes, chronic kidney disease, high blood pressure and other lung conditions, such as pulmonary fibrosis and pulmonary hypertension. Further, depression and anxiety are more prevalent among people with obstructive respiratory disease compared to control groups without respiratory disease.
However, much less is known about the cooccurrence of other psychiatric conditions that are common in U.S. veterans, such as post-traumatic stress disorder (PTSD), substance-use disorders and suicidal thoughts and behaviors.
To address those gaps, researchers led by Patricia M. Bamonti, PhD, of the VA Boston Healthcare System conducted secondary data analyses examining the epidemiology of obstructive respiratory disease in a large, contemporary, nationally representative sample of U.S. veterans.
Specific aims were to:
- Estimate the prevalence of obstructive respiratory disease;
- Characterize differences in sociodemographic, military characteristics and trauma history in veterans with obstructive respiratory disease relative to veterans without obstructive respiratory disease (controls); and
- Compare the prevalence of psychiatric and physical health conditions in veterans with obstructive respiratory disease relative to controls.1
The analyses were conducted using cross-sectional data from the 2019-2020 National Health and Resilience in Veterans Study (NHRVS), which surveyed a nationally representative sample of U.S. veterans. Participants self-reported their personal history of 16 medical conditions, including respiratory diseases, by answering the question, “Has a doctor or healthcare professional ever told you that you have any of the following medical conditions? (Yes or No).”
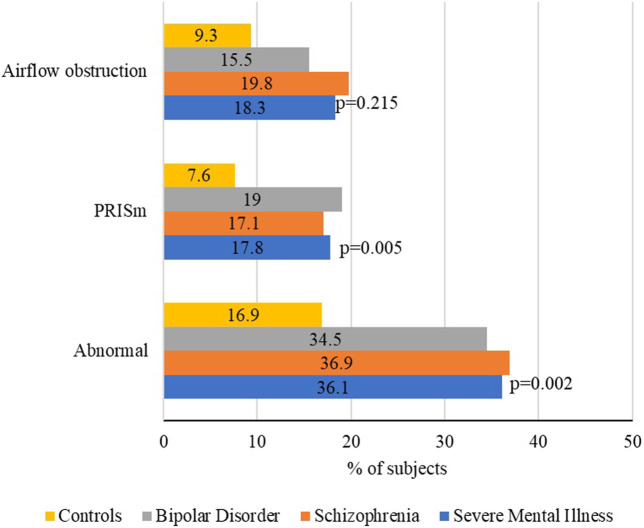
Click to Enlarge: Spirometric patterns. p-values refer to the comparison between serious mental illness and the general population.
Source: Frontiers in Physiology
Participants also completed self-report assessments of other physical health characteristics (e.g., somatic symptoms) and current mental health characteristics (e.g., positive screen for PTSD, current suicidal ideation). Lifetime history of psychiatric and substance-use disorders (major depressive disorder, alcohol-use disorder and drug-use disorder) was assessed using modified self-report versions of the respective modules from the DSM-5 version of the Mini Neuropsychiatric Interview.
A broad range of sociodemographic factors (e.g., age, race/ethnicity, employment status), military characteristics (e.g., combat veteran status) and trauma characteristics (e.g., adverse childhood experiences) were examined as potential correlates of respiratory disease status.
In the sample of 4,069 veterans, those with obstructive respiratory disease were compared to veterans without this disease but who had at least one other medical condition. The comparison focused on sociodemographic, trauma, psychiatric and physical health characteristics. The researchers used multivariable regression analyses to examine the independent associations between obstructive respiratory disease and psychiatric conditions, as well as physical characteristics.
A total of 12.5% of the sample reported a diagnosis of obstructive respiratory disease. Compared to the control group, veterans with this condition were more likely to be female, unmarried/partnered, have lower income, live in the Midwest, receive VA healthcare and have experienced a higher burden of lifetime and childhood trauma, the researchers reported in the Journal of Psychiatric Research.
In adjusted analyses, veterans with respiratory disease had 47-91% higher odds of screening positive for current post-traumatic stress disorder (PTSD), major depressive disorder and generalized anxiety disorder, the researchers reported. They also had 48% higher odds of current suicidal ideation. Additionally, these veterans were more likely to have a lifetime nicotine-use disorder, more medical comorbidities and more severe somatic symptoms. These included arthritis, chronic pain, concussion/traumatic brain injury (TBI), rheumatoid arthritis, kidney disease and osteoporosis or osteopenia.
The researchers stressed that the results of their study should be interpreted in light of limitations. First, a diagnosis of obstructive respiratory disease was self-reported and not confirmed by spirometry and/or medical record review using diagnostic ICD-10 codes, they wrote. Further, veterans were asked to self-report a personal history of obstructive respiratory disease and did not self-report COPD and asthma, which did not allow the researchers to examine asthma and COPD independently. “Although they are both classified as obstructive respiratory diseases, their epidemiology, course, and outcomes differ, with COPD primarily associated with exposure to cigarette smoking and developing in older age, while asthma often occurs earlier in life,” the authors wrote.
Despite these limitations, the current study fills a gap in the literature on the epidemiology of obstructive respiratory disease in U.S. veterans, they wrote. “Our study underscores the importance of the detection and treatment of obstructive respiratory disease and co-morbid psychiatric and medical conditions in this population.”
Another study published in Frontiers in Physiology earlier this year approached the issue from another angle, finding that patients with serious mental illness (SMI), such as schizophrenia and bipolar disorder, have a higher risk of premature morbidity and mortality and lower spirometry values than those without a psychiatric diagnosis.2
The study involved authors from Spanish research institutions and the COPD Foundation in the United States. The authors concluded that “people with SMI have impaired lung function, with up to one-third of them showing an abnormal spirometry pattern. This suggests that regular monitoring of lung function and addressing modifiable risk factors, such as tobacco use and obesity, in this population is of paramount importance.”
They added, “Among natural causes, chronic obstructive pulmonary disease (COPD) is one of the highest causes of excess mortality in people with schizophrenia or bipolar disorder, even higher than that of cardiovascular diseases. In the general population, both COPD and spirometrically determined impaired lung function are associated with increased morbidity and mortality.”
- Bamonti, P. M., Fischer, I., Moye, J., Poghosyan, H., & Pietrzak, R. H. (2024). Obstructive respiratory disease in U.S. veterans: Prevalence, characteristics, and health burden. Journal of psychiatric research, 176, 140–147. Advance online publication. https://doi.org/10.1016/j.jpsychires.2024.05.053
- Ruiz-Rull C, Jaén-Moreno MJ, Del Pozo GI, Gómez C, et. Al. Low lung function in Bipolar Disorder and Schizophrenia: a hidden risk. Front Physiol. 2024 Apr 25;15:1335798. doi: 10.3389/fphys.2024.1335798. PMID: 38737830; PMCID: PMC11084671.

