SALT LAKE CITY—A new study is likely to change treatment patterns for veterans diagnosed with bacterial pneumonia.
New research suggests that using antibiotics that target antibiotic-resistant bacteria as a first-line therapy for pneumonia appears to be unnecessary in most cases.
The report in JAMA Internal Medicine advised that, based on the study of more than 88,000 veteran inpatients with pneumonia, clinicians should reconsider the approach, if they use it. (The pneumonia cases were not related to COVID-19).
University of Utah Health and VA Salt Lake City Health Care System researchers, found that administering empirical anti–methicillin-resistant Staphylococcus aureus therapy for patients hospitalized with pneumonia didn’t make much difference in terms of 30-day mortality.
“Sometimes in our eagerness to improve outcomes, particularly among critically ill patients, we, as doctors, may be overly broad in our initial treatments. This appears to be true with pneumonia, where we found no benefit associated with use of the so-called big gun antibiotics as an initial treatment to cover resistant organisms, even among those patients who are at high risk for these types of infections,” explained senior author Matthew Samore, MD, a University of Utah Health professor of medicine and director of the Informatics Decision Enhancement and Analytic Sciences Center at the VA Salt Lake City Health Care System.
Pneumonia is the leading cause of death from infection in the United States, according to background information in the article. Because causative pathogens are rarely identified, uncertainty remains about the choice of empirical antibiotic therapy.
“For patients hospitalized for community-onset pneumonia, this uncertainty has been magnified by the emergence of resistant organisms, chiefly methicillin-resistant Staphylococcus aureus and Pseudomonas aeruginosa,” the authors explained. “The concept of health care–associated pneumonia, intended to assist clinicians in risk assessment, likely contributed to the overuse of broad-spectrum antibiotics. Consequently, although fewer than 5% of hospitalized patients have resistant organisms detected, more than one-third receive broad-spectrum antibiotics.”
The retrospective multicenter cohort study focused on all hospitalizations in which patients received either anti-MRSA or standard therapy for community-onset pneumonia in the Veterans Health Administration healthcare system from Jan.1, 2008, to December 31, 2013.
Researchers also analyzed subgroups of patients, including:
- Those with initial intensive care unit admission,
- MRSA risk factors,
- Positive results of a MRSA surveillance test, and
- Positive results of a MRSA admission culture.
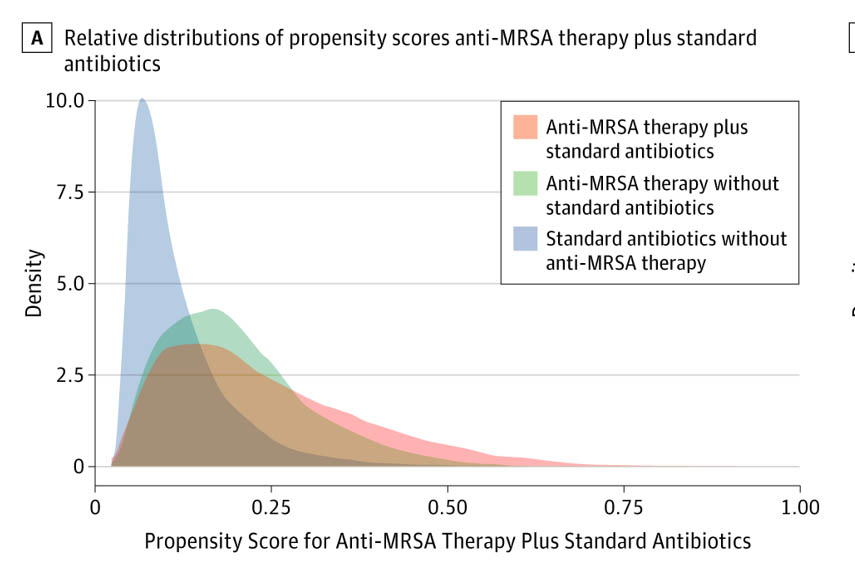
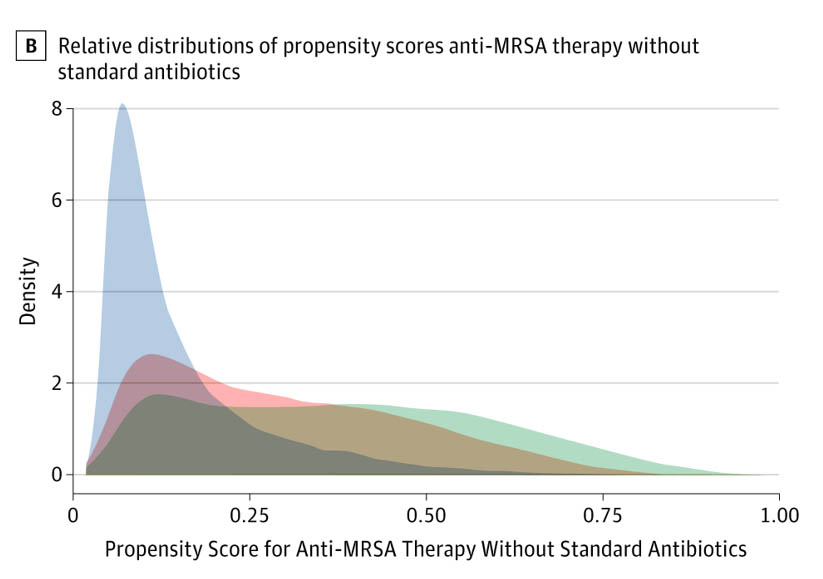
The study sought to determine whether the empirical anti-MRSA therapy plus standard pneumonia therapy vs. standard therapy alone within the first day of hospitalization affected risk of 30-day all-cause mortality after adjustment for patient comorbidities, vital signs and laboratory results. Included in the study were 88,605 hospitalized patients with a median age of 70 years. Empirical anti-MRSA therapy was administered to 33 632 (38%); 10% of them died within 30 days.
Secondary outcomes were defined as the development of kidney injury and secondary infections with Clostridioides difficile, vancomycin-resistant Enterococcus species, or gram-negative bacilli.
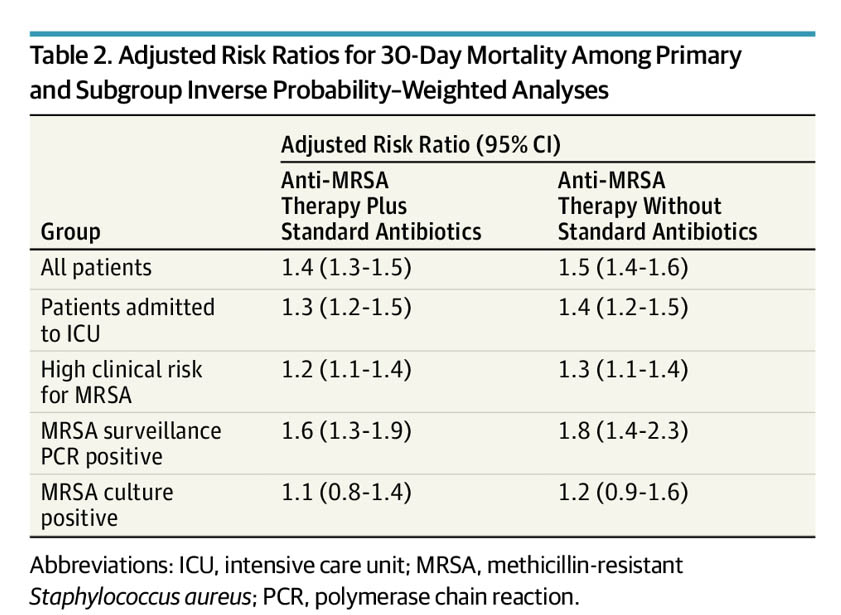
Results of weighted propensity score analysis indicated that, compared with standard therapy alone, empirical anti-MRSA therapy plus standard therapy was significantly associated with an increased adjusted risk of death (adjusted risk ratio [aRR], 1.4 [95% CI, 1.3-1.5]), kidney injury (aRR, 1.4 [95% CI, 1.3-1.5]), and secondary C difficile infections (aRR, 1.6 [95% CI, 1.3-1.9]), vancomycin-resistant Enterococcus spp infections (aRR, 1.6 [95% CI, 1.0-2.3]), and secondary gram-negative rod infections (aRR, 1.5 [95% CI, 1.2-1.8]).
The study found similar associations between anti-MRSA therapy use and 30-day mortality using instrumental variable analysis (aRR, 1.6 [95% CI, 1.4-1.9]) and among patients admitted to the intensive care unit (aRR, 1.3 [95% CI, 1.2-1.5]), those with a high risk for MRSA (aRR, 1.2 [95% CI, 1.1-1.4]), and those with MRSA detected on surveillance testing (aRR, 1.6 [95% CI, 1.3-1.9]).
No Favorable Association
In fact, researchers asserted, “No significant favorable association was found between empirical anti-MRSA therapy and death among patients with MRSA detected on culture (aRR, 1.1 [95% CI, 0.8-1.4]).”
The researchers observed that, as awareness of MRSA infection in the lungs grew, clinicians became more likely to use anti-MRSA therapies as an initial treatment, despite the fact that the resistant condition only accounts for about 2% of pneumonia cases. Use of the more powerful antibiotics rose from about 20% of patients in 2008 to nearly half of them in 2013, according to the study, which suggested that many of the patients who were treated with anti-MRSA antibiotics probably didn’t need them.
The researchers found no discernable benefit of anti-MRSA treatment in addition to standard treatment. In fact, anti-MRSA treatment was associated with a 40% higher risk of dying within 30 days of discharge. Part of the reason might have been potentially severe side effects of vancomycin including increased incidence of kidney failure and secondary infections, according to the authors, who add that further study is needed to fully determine the underlying causes of the increased risk.
With their study suggesting that empirical anti-MRSA therapy was not associated with reduced mortality for any group of patients hospitalized for pneumonia, researchers point to a “growing body of evidence that questions the value of empirical use of anti-MRSA therapy using existing risk approaches.”
“Our study calls into question the strategy of broad empiric antibiotic coverage that has previously been promoted by pneumonia practice guidelines,” explained lead author Barbara Jones, MD, a U of U Health assistant professor of internal medicine, and career development awardee of VA Health Research & Development Service. “We’re not saying that it’s never appropriate to use anti-MRSA therapy for treating pneumonia. But in the absence of better tests to identify MRSA as a potential pathogen causing the disease, using anti-MRSA therapies does not seem to offer any advantage over standard treatment therapy.
“Under these circumstances,” she added, “it may be safer for patients if physicians stick to standard antibiotic treatments for a couple of days to see how patients are doing, rather than leaping into anti-MRSA therapy right off the bat.”
- Jones BE, Ying J, Stevens V, et al. Empirical Anti-MRSA vs Standard Antibiotic Therapy and Risk of 30-Day Mortality in Patients Hospitalized for Pneumonia [published online ahead of print, 2020 Feb 17]. JAMA Intern Med. 2020;10.1001/jamainternmed.2019.7495. doi:10.1001/jamainternmed.2019.7495

