SAN FRANCISCO — VA researchers investigating risk factors for Parkinson’s disease (PD) have identified a strong link between the progressive brain disease and post-traumatic stress disorder (PTSD).
The researchers, whose work has focused largely on the link between environmental toxin exposure and Parkinson’s disease (PD) risk, conducted a retrospective cohort study to explore the association between PTSD and PD. This study involved two groups of veterans who were stationed at Camp Lejeune, NC, and Camp Pendleton, CA, between 1975 and 1985, previously identified for an earlier study.
Out of the 340,489 veterans in the two groups, the researchers identified 158,122 who had used VA healthcare services until Feb. 17, 2021, and/or had Medicare claims through Dec. 31, 2018. They analyzed the veterans’ electronic medical records for diagnoses related to PTSD or Parkinson’s disease (PD). Using a nested case-control study design, they matched 10 control subjects to each veteran with PD based on sex, race and rank. PTSD was found in 15.1% of veterans with PD and in 12.6% of the matched control group.1
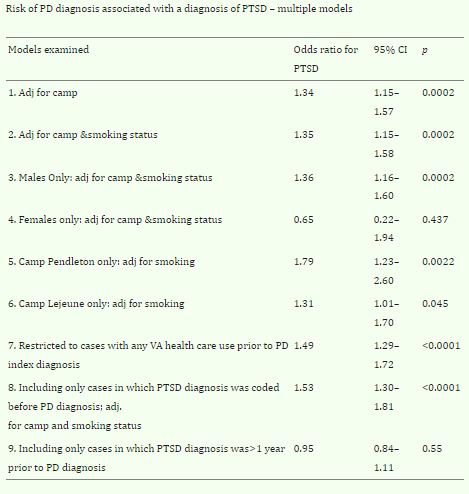
After adjusting for smoking (which has been associated with a reduced risk of PD) and camp where they were stationed, (veterans at Lake Lejeune were exposed to toxins including perchloroethylene (PCE) associated with increased risk), the researchers found that a PTSD diagnosis was associated with a 35% higher risk of PD. If PTSD was coded before Parkinson’s, the increase was 53%, suggesting that PTSD may be a risk factor for PD, the authors wrote.
Although the analysis suggested the risk was higher if PTSD was coded before Parkinson’s, study author Samuel Goldman, MD, MPH, said it is difficult to say with any high certainty when a diagnosis of PTSD occurred. “We think that in most veterans with PTSD, the PTSD probably relates to events that occurred during military service, and Parkinson’s generally a disease of later in life,” he told U.S. Medicine.
While several studies have suggested a connection between PD and PTSD, those studies have based a diagnosis of Parkinson’s solely on ICD codes, which aren’t always reflective of actual cases, explained Goldman, a professor in the Departments of Medicine and Neurology at the University of California, San Francisco (UCSF) and a principal investigator in the San Francisco VAMC.
Better Accuracy
In contrast, the new study, which was published in the Journal of Parkinson’s Disease, identified cases using a combination of ICD codes and/or use of PD medications and validated diagnoses by chart review to better ensure accuracy. From the list of 1,095 cases with a PD ICD code, the researchers’ chart reviews validated a diagnosis of PD in only 430, or 39% of cases, Goldman said.
The study can’t explain why PTSD would precipitate PD, but the researchers suggested a likely reason is stress. “Stress is bad for every disease. It is bad for every organ. It is bad for your heart, it’s bad for your kidneys, and it’s bad for your brain,” Goldman said. “The specific mechanism is probably related to inflammation, but it can also be related to increases in metabolic demands on certain parts of the brain and particularly on substantia nigra and striatum,” he continued. “Those parts of the brain have high metabolic needs, and so they’re particularly susceptible to all sorts of stressors. Anything that tends to overdrive the metalogic needs of this part of the brain is probably harmful.”
For now, the study’s most important message for clinicians is to monitor patients for PTSD and ensure that it is treated effectively. “We feel that early identification and treatment of PTSD can only help,” said corresponding author Frances M. Weaver, PhD, MA, a research health scientist with the Center of Innovation for Complex Chronic Healthcare (CINCCH), Hines VA Hospital in Hines, IL, “The belief is, if you treat PTSD effectively, that perhaps that will reduce the risk of Parkinson’s,” she said, acknowledging further studies are need to confirm that.
In the long term, the researchers said they hope this and other studies on Parkinson’s risk will lead to the development of a risk calculator, much like the Framingham study did for heart disease. “I can imagine that having a diagnosis of PTSD would be something you could build into that calculator for addressing an individual’s lifetime risk of having PD,” Goldman said.
While there are no preventive treatments for PD at present, Goldman says such drugs are on the horizon, and when approved, they will need to be started as soon as possible. “By the time people develop symptoms of Parkinson’s disease, they have already lost about 75% of the neurons in this particular part of the brain,” Goldman said. “So at that point it is unfortunately too late to start protective drugs.”
Thus, a better understanding of the risk factors—including PTSD—could help physicians identify candidates for preventive treatments for PD while there is still time for them to make a difference.
- Weaver FM, Cao L, Stroupe KT, Gonzalez B, et al. Post-Traumatic Stress Disorder and Risk of Parkinson’s Disease in a Veteran Cohort. J Parkinsons Dis. 2024;14(6):1265-1269. doi: 10.3233/JPD-240098. PMID: 39177610; PMCID: PMC11380227.