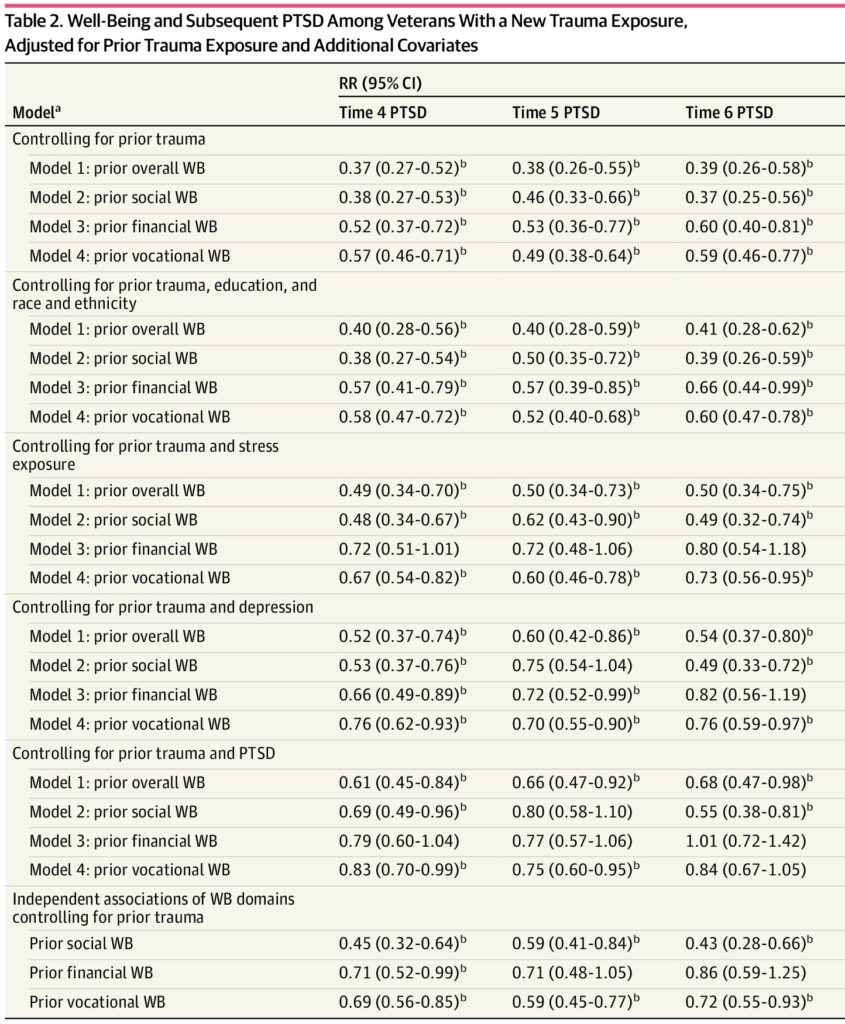
Click to Enlarge: Well-Being and Subsequent PTSD Among Veterans With a New Trauma Exposure, Adjusted for Prior Trauma Exposure and Additional CovariatesAbbreviations: PTSD, posttraumatic stress disorder; RR, risk ratio; WB, well-being.
a. Prior indicates that the characteristic was measured at time point prior to PTSD measurement. In models labeled 1 to 4, only 1 WB factor was entered in the model at a time. In the model examining independent associations of WB domains, all 3 WB domains were entered together in a single model. Some individuals reported trauma at multiple time points and were included in more than 1 time frame in replication analyses. To evaluate whether this might have introduced bias, sensitivity analyses were conducted that removed individuals with multiple reports of trauma, so they were only included in the first time frame that they reported trauma. Because results remained largely similar and the interpretation of findings did not change, the more fully powered analyses appear in this table.
b. P < .05. Source: JAMA Network Open
BOSTON — Victims of traumatic events with higher well-being in three areas—vocational well-being, financial well-being and social well-being—are less likely to experience post-traumatic stress disorder (PTSD), according to a recent study.
The study published in JAMA Network Open investigated whether individuals with higher pre-trauma vocational well-being, financial well-being and social well-being were less likely to experience PTSD following traumatic events. Study authors are affiliated with VA Boston (MA) Healthcare System.1
“Because most people will experience at least one traumatic event in their lifetime (at least 70%), it is important to identify factors that can increase or decrease their risk for developing PTSD, a mental-health condition that can result from trauma exposure,” Dawne Vogt, PhD, a research health scientist at VA Boston Healthcare System, told U.S. Medicine. “Yet, to date most research has focused on identifying factors that increase rather than decrease risk for PTSD, and most of these factors are historical factors that are difficult to intervene on.”
“In this study, my colleagues and I wanted to look at the question of whether veterans’ broader well-being at the time of a traumatic event might influence their risk of developing PTSD, with the idea that, if findings suggest that doing well in other aspects of one’s life is protective against PTSD (which is what we found), this would point to the value of greater investment in well-being promotion efforts for this population and potentially other populations as well,” Vogt explained.
The authors used data from the Veterans Metrics Initiative Study, a large national study of U.S. veterans who completed biannual surveys during the first 3 years after discharge (2016-2019). Using the Well-Being Inventory, a validated measure of psychosocial well-being, the participants reported on their vocational well-being, financial well-being and social well-being.
The study, which included 978 veterans (773 or 79.0% men, mean age of 33.0 years), also assessed the veterans’ experiences of probable PTSD, prior trauma exposure, educational attainment, race and ethnicity, stress exposure, probable depression, and preexisting probable PTSD. The investigators used data from four time points that used the same probable PTSD measure, and they completed statistical analyses.
“Findings revealed that veterans who were doing better with regard to their vocational, financial and especially social circumstances at the time they experienced a new trauma were less likely to develop post-traumatic stress disorder,” Vogt pointed out. “That is, veterans who had jobs they were doing well in and found meaningful, had sufficient financial resources to meet their needs and who reported having satisfying social relationships were less likely to develop PTSD when exposed to a traumatic event. This finding supports the potential value of well-being promotion efforts to reduce risk for PTSD among populations like the military veterans that were the subject of this study.”
The researchers also found that nearly all associations between overall and domain-specific measures of well-being and probable PTSD remained significant and similar in magnitude when accounting for education, race and ethnicity and stress exposure. In addition, they reported that, after adjusting for probable depression, overall well-being associations remained significant, and all domain-based measures were associated with probable PTSD in at least two time frames.
In the healthcare setting, most of the support offered to veterans has focused on treating disease, rather than promoting well-being, Vogt explained. The study’s results provide evidence of the protective role that pre-trauma psychosocial well-being might offer in reducing risk for PTSD.
“This study highlights the need for an expanded focus on well-being, with the goal of preventing disease,” she advised. “This can be accomplished by identifying veterans who would benefit from additional support to improve their vocational, financial and social well-being and connecting them with supports as early as possible to avoid the development of PTSD and other negative outcomes.”
The results support investment in well-being promotion among populations at risk for poor health and highlight the value of focusing these efforts on how well individuals are doing in key roles and activities, according to the investigators.
The study underscored the value of evaluating veterans’ well-being regarding multiple aspects of their life circumstances and connecting veterans who report poor well-being with the supports they need before these challenges can translate into greater risk for PTSD and other negative longer-term outcomes, Vogt pointed out.
Some limitations of the study include dependence on self-reported PTSD measurement and use of an observational rather than experimental design. However, the study has increased confidence in the protective role of psychosocial well-being based on replication of findings, the authors explained.
- Vogt D, Borowski S, Kumar SA, Lee LO, Schnurr PP. Psychosocial Well-Being at the Time of Trauma Exposure and Risk of PTSD. JAMA Netw Open. 2024 Oct 1;7(10):e2440388. doi: 10.1001/jamanetworkopen.2024.40388. PMID: 39453662; PMCID: PMC11512332.

