Cholesterol Drug Use Linked to 25% Reduced Risk of All-Cause Death
BOSTON – In recent years, increased focus has been on deprescribing preventive medication for older patients. The concern has been polypharmacy and related risks from taking too many drugs.
But what if some of the medications still are providing significant benefit, even in users 75 and older?
That was the question tackled in a recent study from the VA Boston Healthcare System and Brigham and Women’s Hospital, both in Boston.
The report in the Journal of the American Medical Association pointed out that research persistently has found that statins can prevent heart attacks, strokes and death in middle-aged adults. Yet, the authors reveal, only 2% of participants in 28 major clinical trials of statins were 75 years or older.1
[Click Image to Enlarge]
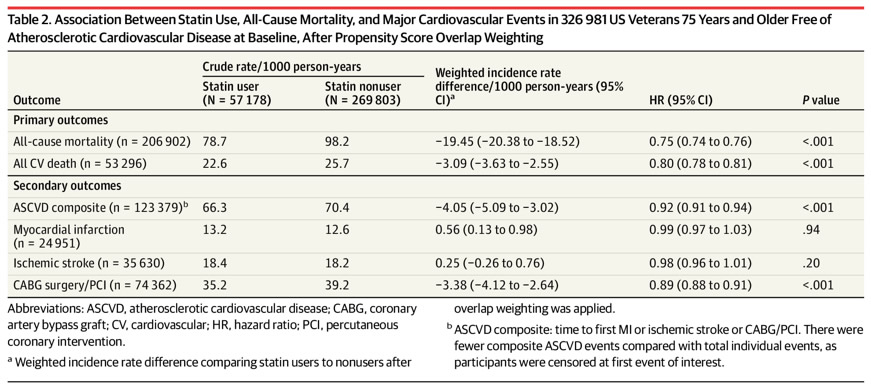
Association Between Statin Use, All-Cause Mortality, and Major Cardiovascular Events in 326 981 US Veterans 75 Years and Older Free of Atherosclerotic Cardiovascular Disease at Baseline, After Propensity Score Overlap Weighting
In light of that, reviewers reviewed VA data, finding that patients who had not yet experienced a heart attack, stroke or other cardiovascular event had a 25% lower risk of dying from any cause if they were treated with statins compared to those who were not. In addition, the risk of dying from a cardiovascular event, such as a heart attack or stroke, was lower by 20%.
“Based on these data, age is not a reason to not prescribe statins,” said lead and corresponding author Ariela Orkaby, MD, MPH, a physician scientist at VA Boston Health Care System and in the Division of Aging at the Brigham . “Statins are commonly studied and prescribed for middle-aged adults but understudied in people over age 75. One of the most remarkable things about our results is that we found the benefit of statins held true regardless of whether a person was older or younger or had a condition such as dementia.”
Defined as primary outcomes in the retrospective analysis were all-cause and cardiovascular mortality. Secondary outcomes included a composite of atherosclerotic cardiovascular disease events, including myocardial infarction, ischemic stroke, and revascularization with coronary artery bypass graft surgery or percutaneous coronary intervention.
Of 7.2 million veterans, 75 and older, seen at the VHA between 2002-2016, 648 677 were determined to have had no prior statin prescription. Of these, 138 055 were excluded because of missing demographic data, 179 428 because of prior ASCVD events, and 4213 because of death in the first 150 days from baseline. Ultimately, 326,981 veterans were deemed eligible for participation in the review.
Researchers noted that 57,178 (17.5%) patients were new users of a statin, and 53,727 had additional prescriptions during follow-up. Another 269,803 never had a statin prescription during follow-up.
Among participants, mean age was 81.1 (SD, 4.1) years (range, 75-107 years), 91.0% were white, and 97.3% were men. The most commonly prescribed statin was simvastatin (84.8%), followed by lovastatin (11.0%), pravastatin (2.5%), and fluvastatin (1.2%). Atorvastatin and rosuvastatin were used by 0.5%.
Veterans initiating a statin were more likely to have diagnostic codes for hyperlipidemia, hypertension, and diabetes. Those in the group were also more likely to have arthritis; polypharmacy; use diuretics, angiotensin-converting enzyme inhibitors, β-blockers, and take non-statin cholesterol-lowering medications; and less likely to have dementia.
ASCVD Deaths Lower
During mean follow-up of 6.8 (SD, 3.9) years, 206,902 patients died, including 53,296 from cardiovascular issues. Researchers report that 78.7 and 98.2 total deaths/1000 person-years among statin users and nonusers, respectively (weighted incidence rate difference [IRD]/1000 person-years, –19.5 [95% CI, –20.4 to –18.5]).
In addition, 22.6 and 25.7 cardiovascular deaths per 1000 person-years occurred among statin users and nonusers, respectively (weighted IRD/1000 person-years, –3.1 [95 CI, –3.6 to –2.6]).
The study advises that, for the composite ASCVD outcome,123,379 events were recorded, with 66.3 and 70.4 events/1000 person-years among statin users and nonusers, respectively (weighted IRD/1000 person-years, –4.1 [95% CI, –5.1 to –3.0]).
After propensity score overlap weighting was applied, according to the authors, the hazard ratio was 0.75 (95% CI, 0.74-0.76) for all-cause mortality, 0.80 (95% CI, 0.78-0.81) for cardiovascular mortality, and 0.92 (95% CI, 0.91-0.94) for a composite of ASCVD events when comparing statin users with nonusers.
“Among U.S. veterans 75 years and older and free of ASCVD at baseline, new statin use was significantly associated with a lower risk of all-cause and cardiovascular mortality,” the researchers emphasized. “Further research, including from randomized clinical trials, is needed to more definitively determine the role of statin therapy in older adults for primary prevention of ASCVD.”
“There are many interesting leads to follow up on,” Orkaby added, “but it’s important to keep in mind that this is not a randomized, clinical trial. Instead, it’s a retrospective analysis using real world data that helps us explore where the truth lies.”
The authors pointed out that their study focused only on veterans, a predominantly white and male population, which could limit its generalizability, although the study’s size enabled it to extract statistically meaningful information on underrepresented groups. Another issue is that, since the study was conducted, higher-dose and higher-intensity statins have become more frequently prescribed, which could affect results, according to the researchers.
Background information in the study pointed out that life expectancy has increased and adults 75 years and older are the fastest-growing segment of the population, explaining, “By 2050 more than 45 million Americans will be 75 years and older, with a proportional rate of increase greatest in those 85 years and older. Incidence and prevalence of atherosclerotic cardiovascular disease (ASCVD) rises with age and remains the leading cause of death, reduced quality of life and increased medical costs. However, although older adults bear the majority of the global ASCVD burden, they are infrequently included in clinical trials that provide the evidence for prevention and treatment guidelines.”
Even those that cohort is under-represented in clinical trials for statins, researchers sate that life tables estimate that an individual who has reached age 80 will live on average eight to nine additional years and could benefit from preventive medications. “This is one reason the updated 2018 cholesterol guidelines recommend statins as a reasonable choice for primary prevention of ASCVD for individuals 75 years and older without a life-limiting disease,” the authors write.
In their review, the authors point out, results remained consistent even at advanced ages and in those with comorbidities. They noted that similar lower risk for mortality was observed in statin users 90 years and older or with dementia.
- Orkaby AR, Driver JA, Ho YL, et al. Association of Statin Use With All-Cause and Cardiovascular Mortality in US Veterans 75 Years and Older. 2020;324(1):68-78. doi:10.1001/jama.2020.7848


