Concurrent Use Raises Overdose Risks
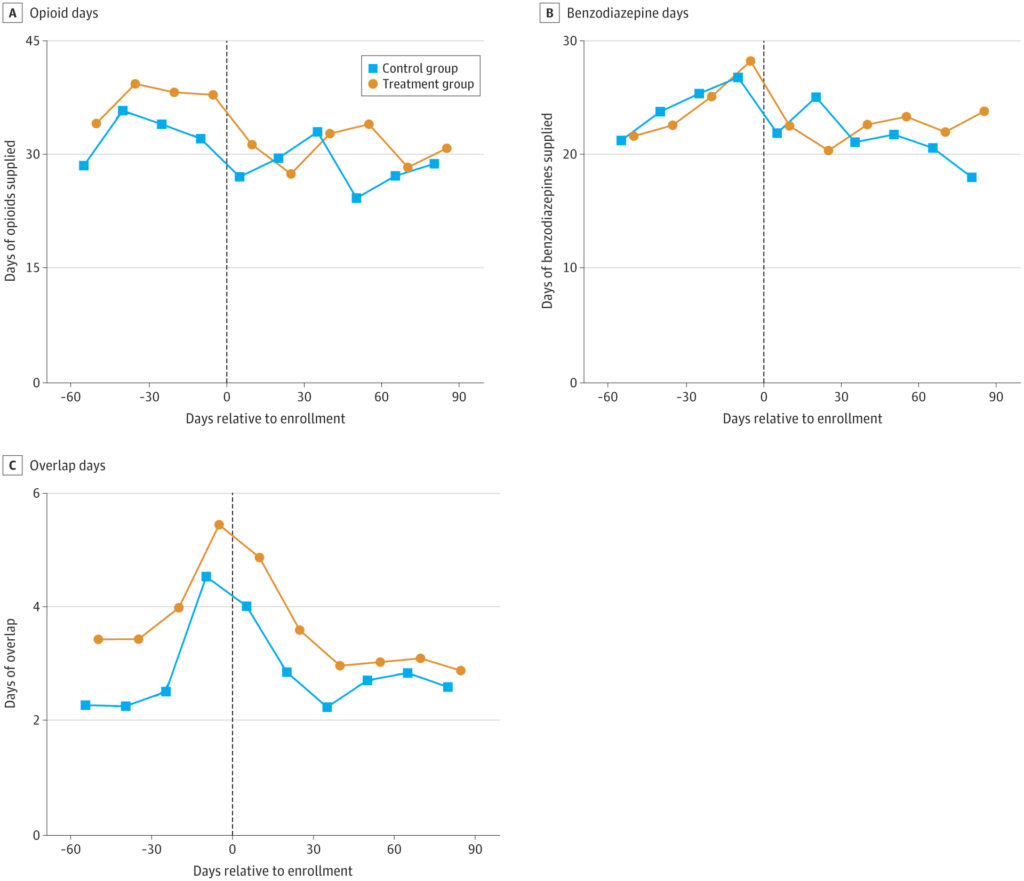
Click to Enlarge: Each point represents the average days of drug supplied by practitioners in the control group and treatment group during a 15-day period relative to enrollment, defined as the date their first patient was enrolled in the study. Practitioners allocated to control or treatment group according to the assignment of their first patient enrolled in the study. Averages use inverse probability of treatment weights based on the allocation ratio at the time of enrollment. Each panel considers the days of opioids, benzodiazepines, and overlapping opioids and benzodiazepines, respectively, the practitioner supplied during the period. Overlapping opioid and benzodiazepine days defined as the number of patient-days to which the practitioner contributed. The vertical line denotes the day of enrollment. Source:
NEW YORK — Email alerts sent from pharmacists to practitioners who prescribe opioids and benzodiazepines fail to reduce concurrent prescribing of these medications, which can put patients at risk of overdose, according to a new study.
The randomized clinical trial published in JAMA Health Forum investigated whether pharmacist emails to practitioners caring for patients who recently received opioids and benzodiazepines reduced co-prescribing of these medications.i
Study participants were patients in the MHS’ National Capital Region (NCR) and their associated NCR practitioners, defined as their opioid prescribers, benzodiazepine prescribers and primary care manager. In the randomized clinical trial conducted from 2019 to 2021, 2,237 patients who had received both opioids and benzodiazepines, as well as 789 clinicians were involved.
To meet the criteria, the patient needed at least one opioid-benzodiazepine overlap day in the last month, according to their dates of service and days’ supply of their prescription drug fills. Patients also were required to have at least one practitioner eligible for emails. The study required at least two practitioners for the first 421 patients. Patients who were receiving hospice care, had a cancer diagnosis or were under the age of 18 were excluded from enrollment, as were those who had already been enrolled.
The researchers focused on these patients because taking opioids and benzodiazepines together can increase the risk of overdose. The study used the Military Health System Population Health Portal Opioid Management Registry to find patients for the study. The registry contains nearly real-time data on prescribing in the MHS.
In the study, clinical pharmacists sent an email alert to practitioners informing them that their patient may be at risk for a life-threatening opioid-benzodiazepine interaction. The messages were standardized and designed to facilitate coordination between practitioners, increase awareness of guidelines, and provide action steps and resources.
“We were not able to detect an effect of the emails on prescribing of opioids or benzodiazepines,” Adam Sacarny, PhD, assistant professor of health policy and management in the Columbia University Mailman School of Public Health in New York, told U.S. Medicine. “Or, put another way, the effect of the emails was not statistically significant. While this result is not what we hoped for, it’s also useful and important, because it shows that the resources devoted to the email alerts can be moved to other efforts to make patient care better and safer.”
Overall, the email alerts didn’t significantly affect patient receipt of these medications or practitioner prescribing, according to the study.
During the past two decades, opioid overdoses and deaths have increased substantially, becoming a public health crisis. Harms to patients from benzodiazepines have been similar, but have received less publicity. One-third to one-half of prescription opioid overdose deaths involve a benzodiazepine. In 2017, more than 1 in 5 patients prescribed an opioid also received a benzodiazepine. Though this rate has declined in recent years, three million adults still receive concurrent prescriptions annually, the study reports.
Risky Prescribing
The study’s findings highlight the importance of improving the quality and safety of healthcare for patients. Concurrent prescribing of opioids and benzodiazepines can be risky for patients, because benzodiazepines can worsen respiratory depression from opioids, which is the cause of opioid overdose. Prescribing guidelines warn about the risks of prescribing opioids and benzodiazepines together, Sacarny explained in an email.
Recommendations to avoid the co-prescribing of these medications appear in guidelines from the national Centers for Disease Control and Prevention, the VA and DoD’s joint guidelines, Choosing Wisely guidance from the American Society of Anesthesiologists and the Beers Criteria from the American Geriatrics Society. The U.S. Food and Drug Administration also requires black-box warnings about overdose on all opioid and benzodiazepine product labeling.
This randomized clinical trial didn’t determine whether certain types of practitioners or those with particular demographics were more likely to concurrently prescribe opioids and benzodiazepines.
Since pharmacist emails probably won’t have a significant effect on the prescribing of these medications, the study emphasizes the value of testing and learning to make opioid and benzodiazepine prescribing safer.
“I think this research shows the value of embedding rigorous testing into quality improvement efforts,” Sacarny wrote. “The Department of Veterans Affairs and the Military Health System have conducted rigorous QI evaluations, including but definitely not limited to this one. This work helps veterans and servicemembers who use these systems, as well as the clinicians who work in these systems. The findings from these efforts are beneficial to patients and professionals even when they suggest interventions are not effective because they create opportunities to focus on more useful work to make health care safer.”
To learn what makes prescribing safer, it’s important to build evaluation into prescribing quality improvement efforts, Sacarny added.
“As for specific interventions, it’s clear that over time, the riskiest opioid prescribing has become a lot less prevalent in the U.S. healthcare system,” Sacarny wrote. “These developments point to new prescribing guidelines and efforts to promote them, changes in prescribing “defaults” (including making the default duration of prescriptions shorter), and better access to information through prescription monitoring programs.”
- Sacarny A, Safran E, Steffel M, Dunham JR, et. al. Effect of Pharmacist Email Alerts on Concurrent Prescribing of Opioids and Benzodiazepines by Prescribers and Primary Care Managers: A Randomized Clinical Trial. JAMA Health Forum. 2022 Sep 2;3(9):e223378. doi: 10.1001/jamahealthforum.2022.3378. PMID: 36218952; PMCID: PMC9526090.

