Click to Enlarge: Oral vs Intravenous Antibiotics for Fracture-Related Infections. Source: JAMA Network
NASHVILLE, TN — Both oral and intravenous antibiotics are effective after fracture-related infection (FRI), a serious complication following fracture fixation surgery, according to a recent study.
The study published in JAMA Surgery evaluated the effectiveness of treatment of FRI with oral versus IV antibiotics.1
Study authors are affiliated with the Major Extremity Trauma Research Consortium (METRC), which unites more than 80 trauma centers across the United States and Canada that are dedicated to advancing care standards for patients with severe extremity trauma. Brooke Army Medical Center at Fort Sam Houston, TX, and the
Naval Medical Center, Portsmouth, VA, both participated in the study.
FRI is a common and serious complication following fracture fixation surgery, particularly for open fractures, which are common in civilian and combat-related injuries. Developing an infection prolongs recovery and increases the risk of nonunion, amputation, sepsis and death, the researchers explained.
The investigators wanted to compare oral versus intravenous antibiotics following FRI, because oral antibiotics are much less expensive, more convenient for patients and do not have complications of line infection or clotting, William T. Obremskey, MD, MPH, MMHC, professor of orthopedic surgery, director of the Orthopedic Trauma Fellowship and director of the Division of Orthopaedic Trauma Research at Vanderbilt University Medical Center, told U.S. Medicine. Current treatment of FRIs involve debridement and six weeks of IV antibiotics, the study reported.
This research area also was of interest because FRIs are a major issue in military personnel, and some severe military injuries have had a 40% infection rate, Obremskey pointed out.
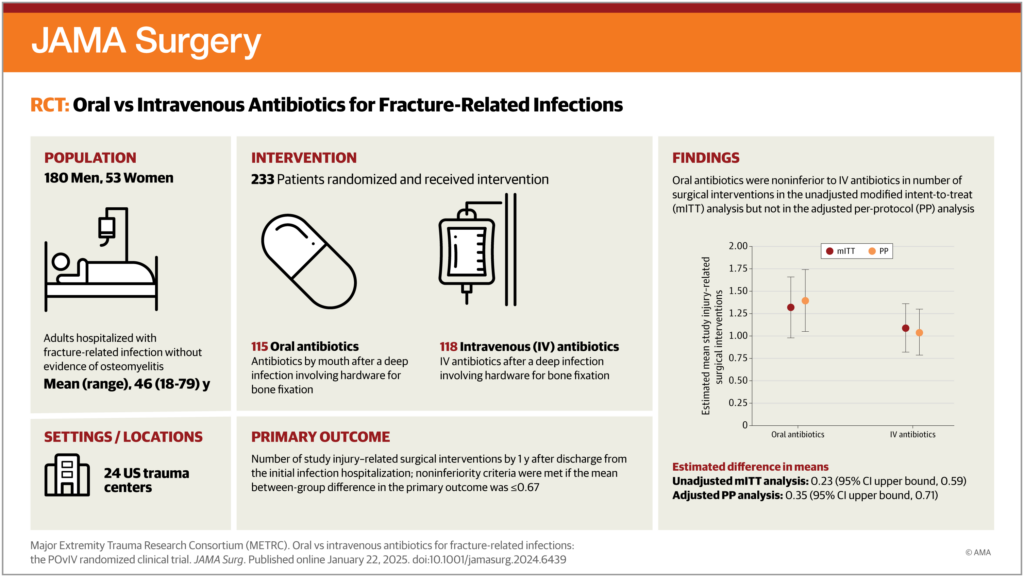
The multicenter, prospective randomized clinical trial was conducted across 24 U.S. trauma centers. Patients included in the study, aged 18 to 84 years old, had fracture repair or arthrodesis with fixation with implants and developed an FRI without radiographic evidence of osteomyelitis, according to the investigators.
The 233 patients were enrolled between March 2013 and September 2018 and followed up for 12 months after hospitalization for treatment of their FRI. The mean age of patients was 46.0 years old, with 53 patients (22.7%) being female and most patients being male (180 patients or 77%). The largest subgroup of patients was in the tibia or fibula group (64.4%), followed by femur (6.9%) and radius or ulna (6.9%) fractures.
The primary outcome of the study was a number of surgical interventions within one year after discharge from the initial infection hospitalization. A key secondary outcome was the recurrence of a deep surgical site infection requiring surgical treatment by one year, which was determined by a masked panel of three orthopedic surgeons. Additional secondary outcomes included nonunion between six and 12 months, treatment failure by one year and rehospitalization due to complications of the injury by one year. Deep surgical site infection was defined by modified criteria from the Centers for Disease Control and Prevention (CDC), the authors explained.
“Providers and patients can consider PO or IV antibiotics to be effective for treating infections after bone fixation,” Obremskey said. “Reinfection was similar in all analyses in patients with a bone fracture infection and treated with either IV or PO antibiotics.”
“Reoperation was found to be noninferior in patients treated with PO versus IV antibiotics after an infection of a bone fixed with hardware,” he added.
The authors determined that oral and IV antibiotics appear to have similar results treating infection after fracture surgery with regard to the primary outcome of number of surgical interventions and the secondary outcome of reinfection in the preplanned, unadjusted analysis.
The total number of observed injury-related surgical interventions within one year after discharge from the initial infection hospitalization was 137 in the oral antibiotics group (1.32 interventions per person-years of follow-up; 52 patients had 0 interventions) and 118 in the IV group (1.09 interventions per person-years of follow-up; 56 patients had 0 interventions), according to the study.
Based on the analyses, the estimated mean number of injury-related surgical interventions within one year was 1.32 (95% CI, 1.00-1.66) and 1.09 (95% CI, 0.83-1.36) for the oral and IV antibiotic groups, respectively, the researchers pointed out.
However, the findings are less clear in additional preplanned and post hoc secondary analyses conducted due to crossover and imbalance between randomized groups, study authors suggested.
“We had some imbalance with the patients in spite of randomization,” Obremskey said. “With the per protocol analysis with statistical adjusting, the number of secondary surgeries was higher in the PO group, but reinfection was still similar and noninferior.”
In the study, patients were randomized if cultures indicated organisms were sensitive to available oral or IV antibiotics or if diagnosed with a culture-negative infection. Participants also were randomized if they had no drug allergies or interactions and if the surgeon and infectious disease team determined the patient could be treated using oral or IV antibiotics. Patients randomized to the IV group were permitted to receive adjuvant therapy of oral rifampin and be considered adherent, the study authors explained.
Overall, the researchers concluded that clinicians and patients can use these data to inform shared decision-making regarding antibiotic care for FRIs.
- Major Extremity Trauma Research Consortium (METRC); Obremskey WT, O’Toole RV, Morshed S, Tornetta P 3rd, et. Al. Oral vs Intravenous Antibiotics for Fracture-Related Infections: The POvIV Randomized Clinical Trial. JAMA Surg. 2025 Jan 22. doi: 10.1001/jamasurg.2024.6439. Epub ahead of print. PMID: 39841468.

