Click to Enlarge: Emotional Awareness and Expression Therapy or Cognitive Behavioral Therapy for Chronic Pain in Older Veterans
Source: JAMA Network Open
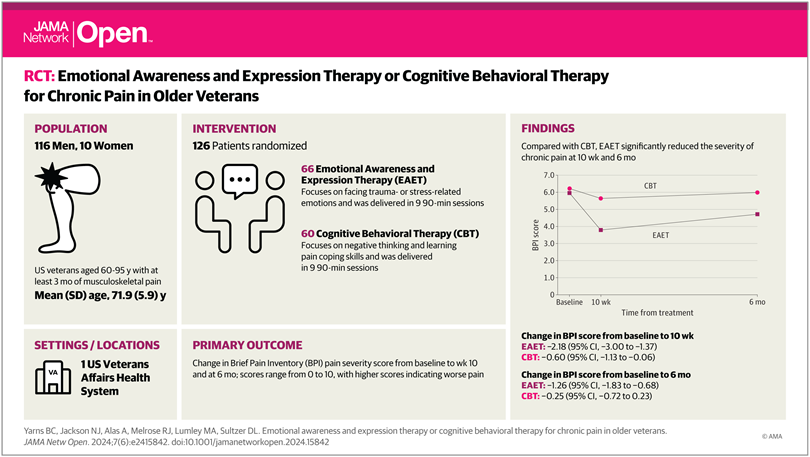
LOS ANGELES — Chronic pain in older adults can be significantly reduced using a newly developed psychotherapy called emotional awareness and expression therapy (EAET), which confronts past trauma and stress-related emotions that can exacerbate pain symptoms, according to a new study.
The randomized clinical trial, published in JAMA Network Open, evaluated whether EAET is superior to traditional cognitive-behavioral therapy (CBT) for treating chronic pain in predominantly male older veterans. The researchers also compared the two psychological therapies in treating mental health symptoms such as depression, anxiety and posttraumatic stress disorder (PTSD) symptoms, which are key targets of EAET, in older veterans.1
Study authors are affiliated with VA Greater Los Angeles (CA) Healthcare System and the University of California, Los Angeles.
Chronic pain, which is “common and disabling in older adults, is a risk factor for cognitive decline and premature death. Medical and surgical interventions, particularly opioids, often produce only partial efficacy and pose substantial risks,” the authors explained.
Psychological interventions “could be a safer option, but CBT, the gold standard approach, provides only modest benefits. Veterans, a vulnerable population, have high rates of severe pain and overlap between pain and psychiatric conditions, such as depression, anxiety and PTSD, which may further limit the effectiveness of CBT. More powerful treatment options are needed,” the researchers suggested.
EAET, a psychotherapy, is a “novel, evidence-based approach to treating chronic pain. In individual or group sessions, EAET targets unresolved trauma or emotional conflicts to reduce or resolve pain symptoms. Randomized controlled studies have shown that EAET is effective for some patients with pain conditions such as fibromyalgia, a condition that involves widespread musculoskeletal pain, along with sleep, memory and mood issues”, lead author Brandon C. Yarns, MD, MS, told U.S. Medicine.
This two-arm randomized clinical trial involved a racially and ethnically diverse group of 126 veterans age 60 to 95 years old with at least three months of musculoskeletal pain, including back, leg or pelvic pain; neck pain or whiplash; temporomandibular joint disorder; fibromyalgia; tension headache; or any combination of these. The trial was conducted in the VA Greater Los Angeles Healthcare System from May 16, 2019, to Sept. 14, 2023.
The veteran patients, 66 in the EAET group and 60 in the CBT group, participated in EAET and CBT, conducted concurrently, with each treatment presented as one 90-minute individual session followed by eight 90-minute group sessions. The mean age of participants was 71.9 years, 116 (92%) were male, 111 (88%) completed posttreatment and 104 (82%) completed the six-month follow-up, study authors reported.
The study found that “older veterans who participated in EAET received statistically significant benefits on every outcome we measured when comparing symptoms from the start to the end of treatment and in a six-month follow-up within the EAET group”, said Yarns, a psychiatrist at the VA Greater Los Angeles Healthcare System and the David Geffen School of Medicine at University of California, Los Angeles.
He noted, “In addition, at posttreatment EAET produced significantly better outcomes than cognitive behavioral therapy (CBT) on pain severity, depression, anxiety, PTSD, general life satisfaction, patient global impression of change and global treatment satisfaction. The differences between the treatments on pain reduction were quite large, as 63% of EAET participants had clinically significant (at least 30%) pain reduction, whereas only 17% of CBT participants met this benchmark. The advantage of EAET over CBT was maintained for pain reduction, depression and global impression of change for six months after the end of treatment.”
The findings “support the superiority of EAET compared with CBT in reducing chronic pain among older veterans,” according to the authors.
Reduced or Eliminated
Most importantly, the randomized clinical trial found that “many cases of chronic musculoskeletal pain may be reduced or possibly even eliminated. Nearly two-thirds of EAET participants in the trial had clinically significant pain reduction, and around 12% had greater than 70% pain reduction at posttreatment. This was in a sample of highly medically and psychiatrically complex older veterans from diverse racial and ethnic backgrounds,” Yarns pointed out, adding, “I hope these findings can renew hope among healthcare professionals for their patients with back pain, neck pain and other musculoskeletal conditions.”
In a UCLA Health press release, Yarns suggested, “Most people with chronic pain don’t consider psychotherapy at all. They’re thinking along the lines of medications, injections, sometimes surgery or bodily treatments like physical therapy. Psychotherapy is an evidence-based treatment for chronic pain. What this study adds is that the type of psychotherapy matters.”
He explained the “goal in CBT is not necessarily to cure pain, but to learn to cope and live well despite chronic pain. Patients with chronic pain undergo treatment with similar exercises to those used to treat depression or anxiety, such as guided imagery, muscle relaxation, cognitive restructuring and activity pacing. The aim is for patients to improve their ability to tolerate their pain.”
On the other hand, “EAET has one primary intervention, which is experiencing, expressing and releasing emotions. EAET aims to show patients the brain’s perception of pain is strongly influenced by stress-related emotions. Patients are asked to focus on a stressful interaction, anything from mundane to severe traumas. Patients experience these emotions both in mind and body and then work to confront these emotions, express their reactions and ultimately let go,” Yarns said.
“If there is a hurt or stressor, people have a series of normal, natural emotional reactions,” he added. “There might be anger, guilt and sadness. Because these feelings are painful, people often avoid them, but EAET helps people face difficult feelings with honesty and self-compassion. In therapy, they can release anger, pain and guilt that they’ve been carrying and are left with self-compassion in the end.”
For healthcare professionals who are treating veteran patients with chronic pain, Yarns recommended “paying close attention to the role of stress and emotions in chronic pain.”
“A great place to start is for healthcare professionals simply to take a history of trauma and stress,” he suggested. “Often, people with chronic pain will report a history of adverse childhood experiences, stressful life events around the time their chronic pain started and exacerbations of their pain that are tied to stress. Just asking about life experiences can help the patient and provider put the pieces together.”
The clinical trial’s results suggest that “EAET may be a preferred intervention for medically and psychiatrically complex patients with pain. Also, incorporating the principles of EAET into mainstream clinical pain medicine could improve the societal burden of chronic pain,” according to the authors.
- Yarns BC, Jackson NJ, Alas A, Melrose RJ, Lumley MA, Sultzer DL. Emotional Awareness and Expression Therapy vs Cognitive Behavioral Therapy for Chronic Pain in Older Veterans: A Randomized Clinical Trial. JAMA Netw Open. 2024;7(6):e2415842. doi:10.1001/jamanetworkopen.2024.15842

