Public health officials across the country have warned that the combination of the COVID-19 pandemic and influenza could endanger a record number of Americans and overwhelm healthcare facilities this fall and winter.
Black, Hispanic Veterans Twice as Likely to Test Positive for COVID-19
Non-Hispanic Black and Hispanic veterans were twice as likely as non-Hispanic white veterans to test positive for COVID-19 at the VA, even after accounting for other demographics, geographic location and underlying health conditions.
Maintenance Rituximab An Option in Some Follicular Lymphoma Cases
SALT LAKE CITY, UT – Since the release of the National LymphoCare Study nearly 10 years ago, few studies have described real-world practice patterns and clinical outcomes in patients with follicular lymphoma, including the use of maintenance rituximab therapy in the...
Humanized Monoclonal Antibodies Show Promise in Relapsed/Refractory CLL
SACRAMENTO, CA – What are the complement depleting effects of humanized monoclonal antibodies and the impact of complement replacement on treatment response in patients with hard-to-treat chronic lymphocytic leukemia? A small phase 2 trial published in the Journal of...
First Line Ibrutinib Delays Time to Next Treatment for Veterans With CLL
HORSHAM, PA -- Chronic lymphocytic leukemia/small lymphocytic lymphoma is the most common adult leukemia, accounting for about 37% of all leukemias in the United States. Yet, a new study suggested that limited real-word evidence is available on the outcomes of...
With COVID-19 Cases Still Climbing, VA Seeks to Improve Telehealth
While the number of COVID-19 cases being actively treated at VA facilities declined, the total number of infections and deaths rose steadily in July and August.
APA Recommends Ongoing Use of Long-Acting Injectables for SMI
WASHINGTON — Even as VA facilities open up nationwide, administrators and others are keeping a wary eye on the possibility of a significant second wave of the COVID-19 pandemic in the fall. U.S. healthcare systems are preparing now for a sharp increase in cases in the...
Study Urges Integration of Co-Morbid Mental Health, Substance Use Treatment
Many mental health programs will not accept patients with active substance use issues. That effectively denies treatment to many veterans who have served in the past 20 years, among whom co-occurring substance use disorders and mental health disorders are particularly common.
Switch to Long-Acting Injectable Reduces VA Costs for Schizophrenia Care
Schizophrenia can be frightening and life-changing. Common symptoms such as disorganized thinking and speech, lack of expressive emotion, social withdrawal, neglect of self-care, hallucinations and delusions alienate individuals with schizophrenia from others and create barriers to day-to-day functioning in society.
Biomarker IDs Veterans at Risk of Poor Skin Cancer Prognosis
The neutrophil-to-lymphocyte ratio (NLR) biomarker is associated with systemic inflammation and poor prognosis in solid tumors.
Study Reveals Risks of Non-Dermatologists Treating Melanoma
Military personnel often have more exposure to sunlight, compared to their civilian counterparts, and that can increase their risk of melanoma.
Some IBD Patients Have Increased Skin Cancer Risk
Past research has cautioned about the risk of skin cancer with use of immunosuppressive medications. Yet, a new study pointed out, there is limited information on repeated basal cell cancer (BCC) occurrences among inflammatory bowel disease (IBD) patients, especially those who use immunosuppressive medications.
VA Pharmacists Advise on Use of Anticoagulation in Severe COVID-19 Cases
While reports in the literature are increasing about high rates of coagulopathy and venous thromboembolism (VTE) among hospitalized patients with coronavirus disease 2019 (COVID-19), there is little guidance on how to treat it or prevent it.
Dementia Rates Increased With Serious Mental Illness
Because VHA provides a continuum of care over the life course, the healthcare system has need to better understand what effect bipolar disorder and schizophrenia have on veterans’ risk of dementia.
Mild TBI Exacerbates Issues for Early Binge Drinkers
Does early adolescent binge drinking (BD) increases the risk for and/or severity of psychopathology in post-9/11 veterans, and how does mild traumatic brain injury (mTBI) affect the risk?
Most At-Risk Veterans Don’t Get Suicide Counseling
Despite all of the focus on preventing suicides in those who have served in the military, a significant proportion of veterans with suicidal ideation do not take advantage of available mental health treatment, according to a new study.
Statins Reduce Risk of Acute Liver Injury in Veterans With HIV or HCV
In 2013, the American College of Cardiology and American Heart Association issued updated guidelines significantly expanding the number of patients who should be considered candidates for statin therapy.
Direct Acting Antivirals Cure More than 90% of Older Patients with HCV
The American Association for the Study of Liver Diseases and the Infectious Diseases Society of America recommend that nearly all patients with chronic hepatitis C virus infection receive treatment with direct-acting antiviral therapy.
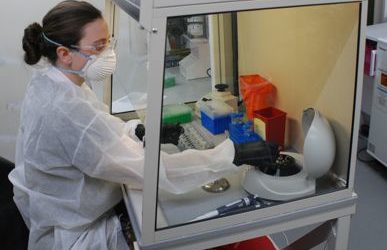
Army Researchers Wage War Against COVID-19 in the Laboratory
As the novel coronavirus has continued to spread throughout the United States, infecting more than six million and killing more than 185,000 people, the U.S. Army has been on the front lines in an effort to protect the nation’s health and security.
COVID-19 Incidence in AI/AN More Than Three Times Greater Than Whites
ATLANTA—Non-Hispanic American Indians and Alaska Natives make up only 0.7% of the United States population but 13% of coronavirus disease cases across the country, according to a new report. The national Centers for Disease Control and Prevention pointed out in an...
‘Happy Hypoxia’ Might Not Be Such a Mystery After All in COVID-19
Earlier in the COVID-19 pandemic, physicians were often baffled by patients who presented with extremely low levels of oxygen. Although oxygenation was so low it was potentially life-threatening in some cases, patients showed no obvious difficulty in breathing.
CLL, Lymphoma Treatments Might Be Effective in Some Melanoma Cases
AURORA, CO – Noting the urgent need to develop treatments for patients with melanoma who are refractory to or ineligible for immune checkpoint blockade, including patients who lack BRAF-V600E/K mutations, a new study suggested some possible options. The report in...
COVID-19 Has Serious Hematological Implications for Many Patients
CHICAGO – Most of the morbidity and mortality seen with COVID-19 involves the lower respiratory track, but the virus also can involve several organ systems and the syndrome. Noting that the novel coronavirus has a wide range of symptoms and manifestations, a report in...
NHL, Some Other Cancers, Reduced With Early ART in HIV-Positive Patients
OAKLAND, CA – Cancer is a significant problem for patients diagnosed with HIV. indicates that earlier initiation of antiretroviral therapy (ART) in persons living with HIV (PLWH) can reduce cancer incidence, but it has not been clear which cancer types are affected. A...
Surveillance, Barriers to Care Key to Federal Medicine Fight Against HCC
Mortality rates from most cancers have declined in recent years, but deaths from hepatocellular carcinoma continue to climb. Both the VA and the DoD are moving aggressively to detect and treat liver disease before it progresses to hepatocellular carcinoma (HCC) and to quickly identify patients who have developed this devastating disease.
New Guidelines Expand Screening for Liver Cancer in NAFLD
The American Gastroenterological Association recently updated its clinical practice guidelines to recommend screening for all patients with nonalcoholic fatty liver disease and cirrhosis.
HCV ‘Cure’ Doesn’t Eliminate Liver Cancer But Might Reduce Mortality
DALLAS – Use of direct-acting antiviral therapy to essentially cure hepatitis C virus does not completely eliminate the risk of developing hepatocellular carcinoma, but recent studies suggest it can significantly reduce mortality rates. The 15% to 20% of HCV patients...
Houston, Miami VAMCs Participate in Tocilizumab Trial
HOUSTON—The Michael E. DeBakey VAMC in Houston and the Bruce W. Carter VAMC in Miami are among nearly 70 locations across the world participating in a randomized double-blind clinical trial of an immunomodulator, tocilizumab, for patients with severe pneumonia...
Foundation Partners with VA to Offer Pandemic Caregiver Relief
WASHINGTON—Providing ongoing care for wounded, ill or injured veterans during ordinary times poses many challenges, but travel restrictions, closures, and childcare issues associated with the COVID-19 pandemic has forced many caregivers to take on additional...
VA Launches COVID-19 Insights Partnership with DOE and HHS
NEW HAVEN, CT—The VA along with the Departments of Energy (DOE) and Health and Human Services (HHS) have established a partnership to share health data, research, and expertise in the battle against COVID-19. VA and HHS will use the DOE’s high-speed computing...