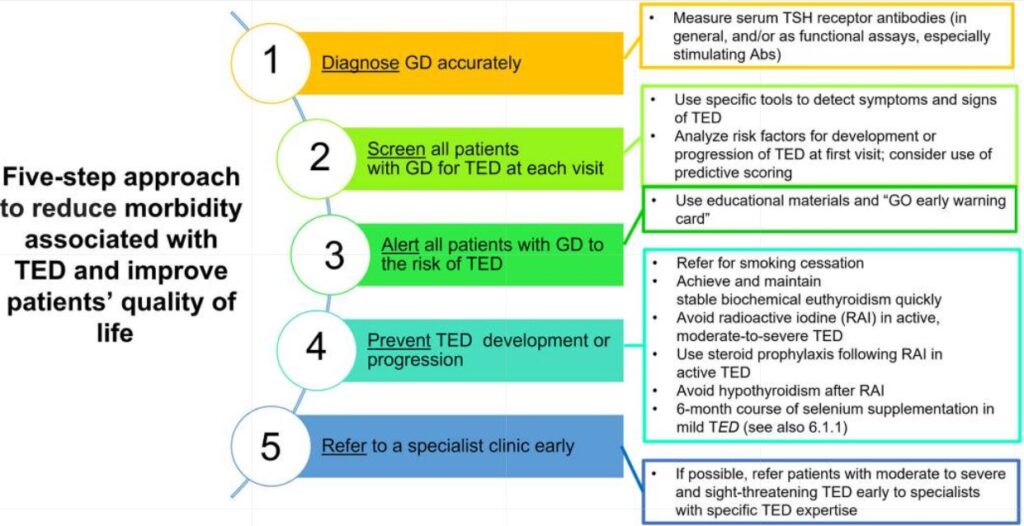
Click to Enlarge: Steps to reduce morbidity and improve quality of life in patients with TED. Measures to reduce morbidity associated with TED and improve patients’ QoL. (This figure is used and adapted with permission, courtesy of the British Thyroid Foundation, from the Thyroid Eye Disease Amsterdam Declaration Implementation Group UK (TEAMeD) (https://www.btf-thyroid.org/teamed-page) and Dr Anna Mitchell. Further description of the Thyroid Eye Disease Amsterdam Declaration is available (17, 20)). Abs, antibodies; GD, Graves’ disease; RAI, radioiodine; TED, thyroid eye disease. Source: European Thyroid Journal
BETHESDA, MD — Also known as Graves’ ophthalmopathy or Graves’ orbitopathy, thyroid eye disease (TED) affects up to a third of people with autoimmune thyroid disease, most commonly hyperthyroidism due to Grave’s disease.
While the condition is usually mild and resolves with time, more severe disease that goes untreated can lead to the expansion of muscle and fat behind the eye, causing disfiguring or debilitating or signs and symptoms such as proptosis (forward protrusion of the eyes), pressure or pain behind the eyes, eyelid retraction and diplopia (double vision) or loss of vision.
Because most patients with TED develop eye manifestations while being treated for hyperthyroidism and under the care of endocrinologists, those specialists have a key role in the diagnosis, initial management and selection of patients who require referral to specialist care. A new consensus statement produced jointly by the American Thyroid Association and European Thyroid Association incorporates the newest treatments into an overview of the management of TED, provides guidance for specialist treating TED emphasizes the need for a multidisciplinary approach—incorporating both the endocrinologist and ophthalmologist—to treating patients with severe TED. The consensus statement was drafted by a multidisciplinary, global writing task force led by co-chairs from both societies. 1
“The TED consensus statement was felt to be needed at this time due to changes in the treatments available for TED,” said Henry B. Burch, MD, program director of the Division of Diabetes, Endocrinology, & Metabolic Diseases at NIH’s National Institute of Diabetes and Digestive and Kidney Diseases who served as chair for the American Thyroid Association.
The most exciting change, he said, is that a new drug, teprotumumab, has been found to effective in reducing some of the most disturbing manifestations including proptosis, inflammatory changes and diplopia. “Clinical trials have shown improved self-reported quality of life in patients treated with teprotumumab,” said Burch, who is also a professor of medicine at the Uniformed Services University of the Health Sciences in Bethesda, MD. He maintains a continuity clinic as a volunteer at the Walter Reed National Military Medical Center, also in Bethesda, and continues to provide guidance and lectures for medical staff, medical students, internal medicine residents, and endocrinology fellows.
The consensus statement, Burch said, is carefully organized into sections dealing with the following:
- Assessment of patients with Graves’ disease and signs or symptoms of TED. Endocrinologists should look for evidence of TED in all patients with Graves’ disease, Burch said. Early assessment and appropriate initiation of or referral for multidisciplinary management is key to improving outcomes from TED.
“A primary objective in the evaluation of TED is to assess factors that inform management and predict outcomes,” the consensus statement states. “Endocrinologists should be familiar with basic elements of a TED examination, enabling assessment of both activity and severity.
Assessment of patients with TED should include activity, severity (with particular attention to impaired ocular motility and visual loss), trend across time, and impact on daily living.”
- Guidance for multidisciplinary management of TED as well as indications and level of urgency of referral to ophthalmology. Endocrinologists managing patients with TED should consider referring them for TED specialty care, according to the consensus statement. Suggested criteria and timing of ophthalmologic referral vary according to clinical presentation of the eye disease, with dysthyroid optic neuropathy, corneal breakdown, globe subluxation and ne diplopia all requiring an urgent referral. Patients with worsening soft tissue changes, an uncertain diagnosis, euthyroid TED (meaning their thyroid is functioning normally), apparently unilateral or markedly asymmetric TED, or significant impact on quality of life should be seen by an ophthalmologist. For others, referral to an ophthalmologist is non-urgent or optional.
- TED management guidance according to activity and severity of disease. “An individualized approach to the management of TED, based on disease activity, severity, duration, trend across time, impact of the disease on daily living, treatment goals, patient age, and comorbidities, as well as the availability and relative costs of therapies, must be advised,” according to the consensus statement. IIn most patients with mild TED, a “watchful monitoring” strategy—including simple measures—is sufficient, although patients with a significant decrease in quality of life can be treated as moderate-to-severe TED.
For disease requiring treatment, different treatment approaches were discussed. Wherever possible, the Task Force members ranked therapeutic approaches as either ‘preferred’, ‘acceptable’, or ‘may be considered.’
- Medical management of TED. The statement provided an in-depth comparison of available medical therapies—and combinations of therapies—including intravenous glucocorticoids, ophthalmic glucocorticorticoids, mycophenolate mofetil, rituximab, teprotumumab and tocilizumab.
Comparisons ranged from efficacy to logistics for delivery to cost to potential adverse effects, said Burch. It also acknowledged the unknowns.
“Even with newer therapy with unprecedented efficacy in clinical trials, there remain a number of unknowns, such as long-term effectiveness and safety. The very high cost and lack of international availability of newer medical therapies for TED remain problematic,” Burch said.
- Surgical management of TED. “Elective surgery to correct proptosis, strabismus, eyelid malposition, and fat pockets can be initiated in inactive TED where clinical stability has been maintained and an euthyroid status achieved before surgery,” according to the consensus statement.
The statement provides more detailed information about different surgeries, when they performed, the order in which they are performed. “Quality of life improvements often occur as a result of surgical rehabilitation for TED,” it states.
- Identification of current research gaps. Despite the availability of new agents and other advancements in the treatment of TED, much remains to be learned about the disease and its management. According to the consensus statement, future research should focus on ways to more simply identify TED or identify those at risk for TED; better ways of assessing TED; the optimal treatment for mild, moderate-to-severe recurrent or refractory TED; the pathogenesis of TED and healthcare models for the management of TED.
A Message for All Clinicians
The consensus statement is designed to provide guidance to endocrinologists, but Graves’ disease is a common problem in both veterans and active military personnel that is likely to be encountered by clinicians in any field. “[Patients] presenting with unexplained weight loss, difficulty sleeping, or palpitations should always have a thyroid blood test,” Burch said.
“Although TED can be diagnosed before Graves’ hyperthyroidism is diagnosed, and some patients with TED never have hyperthyroidism, most cases of TED are diagnosed either concurrently or following the diagnosis of hyperthyroidism,” Burch said. “Therefore, vigilance for TED occurrence must occur in patients diagnosed with thyroid dysfunction.”
- Burch HB, Perros P, Bednarczuk T, Cooper DS, Dolman PJ, Leung AM, Mombaerts I, Salvi M, Stan MN. Management of thyroid eye disease: a Consensus Statement by the American Thyroid Association and the European Thyroid Association. Eur Thyroid J. 2022 Dec 8;11(6):e220189. doi: 10.1530/ETJ-22-0189. PMID: 36479875; PMCID: PMC9727317.

