BIRMINGHAM, AL — Patients with acute myeloid leukemia (AML) face difficult choices if their cancer recurs. Without treatment, survival is a matter of months. The curative treatment at that stage of disease is no sure bet. Hematopoietic stem-cell transplantation, also called blood or marrow transplant or BMT, provides the best option, but not everyone survives its rigors.
Those that do face another set of challenges, a significant impact on their quality of life, which may extend for decades.
In light of the growing number of HCT survivors, a group of researchers recently undertook a comprehensive study of the quality of life of these individuals after transplantation. Donna Salzman, MD, of the Birmingham VAMC and the University of Alabama (UAB), and her colleagues at UAB and other institutions, studied 1,369 AML adult patients who survived for at least two years after HCT between 1974 and 2014 and 1,310 of their siblings. Results of the study were published in the Journal of Clinical Oncology.1
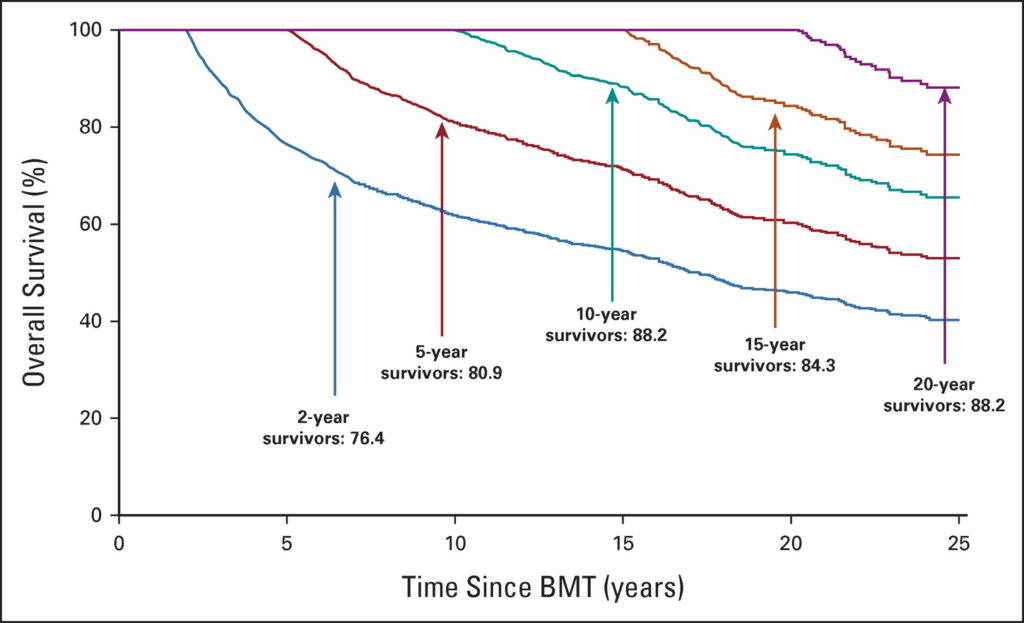
Click to Enlarge: Five-year survival probability stratified on time survived since BMT (≥ 2, ≥ 5, ≥ 10, ≥ 15, and ≥ 20 years) among BMT survivors. BMT, blood or marrow transplantation.
They found that transplantation survivors had a nearly four-fold increase in the odds of severe or life-threatening conditions. Such conditions affected more than half of HCT survivors (54.9%) compared to just over a quarter of their siblings (28.4%), with other neoplasms, diabetes, cataracts, venous thromboembolism and joint replacement among the most prevalent conditions.
In addition, reported poor overall health at a much higher rate and were more likely to have activity limitations and functional impairments. The 20-year incidence of severe, life-threatening, or fatal conditions among transplant survivors was 68%, with chronic graft-versus-host disease associated with higher risk of multiple severe conditions. Relapse-related mortality flattened out at 30% while non-relapse-related mortality rose to 50% by 30 years post-transplant.
“These findings may inform evidence-based health screening recommendations that account for the evolving pattern of morbidity and mortality over time after BMT,” the team wrote. “Our findings support a long-term need for multidisciplinary management of patients with a history of chronic graft-versus-host disease, setting the stage for screening, early detection, and interventions to mitigate risk of adverse health outcomes.”
Another recent study, published in Current Hematologic Malignancy, pointed out that AML survivors face unique challenges affecting long-term outcomes and quality of life, often because of HCT. Yet, wrote the Mayo Clinic-led authors, there isn’t much research on the long-term impact of AML treatment in physical and mental health, disease recurrence, and financial burden in survivors.2
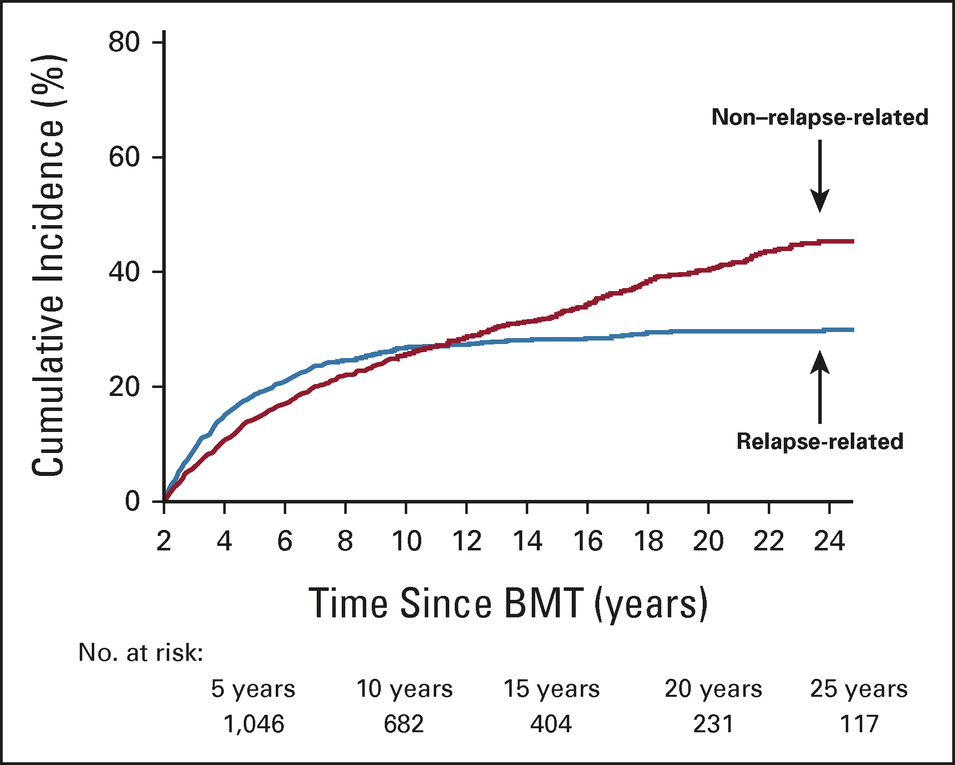
Click to Enlarge: Cumulative incidence of cause-specific mortality among BMT survivors. BMT, blood or marrow transplantation.
“Fatigue, mental health concerns, infections, sexual dysfunction, and increase cancer recurrence occur after AML treatment,” the authors wrote. “Chronic graft-versus-host disease (GVHD) and infections are common concerns in AML after hematopoietic stem cell transplantation (HCT). Survivorship guidelines encompass symptoms and complications but fail to provide an individualized care plan for AML survivors. Studies in patient-reported outcomes (PROs) and health-related quality of life (HRQoL) are sparse.”
Background information in the study pointed out that new AML therapies and allogeneic hematopoietic stem cell transplant (allo-HCT) have led to a growing population of survivors. “Approximately 60–70% of adult patients aged 18–65 will achieve a complete remission, and 30.5% of these adult AML patients have a five year or more overall survival,” the study noted. “From 2009 to 2019, there were an estimated 28,003 AML individuals in the US who have survived 5 or more years following allo-HCT (CIBMTR, 2022). As the population of AML survivors is growing, understanding the most relevant survivorship aspects constitute a key component for routine follow-up care.”
The study team concluded that AML is an aggressive hematologic malignancy and the intensive treatment it requires “profoundly affects survivors HRQOL.” With a growing population of AML survivors, the need to improve survivorship care and to enhance survivors’ overall health, wellness, and QoL increases.
“PCPs and oncologists need to communicate adequately about a patient’s survivorship care plan, which should include surveillance testing for recurrent or subsequent primary cancers, disease prevention, management of comorbid conditions, and monitoring for physical and psychological effects of cancer treatment,’ the authors advised. “Survivors and caregivers need to have resources available to them in how to navigate back into a new normalcy of life, including care for medical complications, coping mechanisms for mental health problems, resources for financial burden, and social reintegration.”
- Armenian SH, Chen Y, Hageman L, Wu J, Burden of Long-Term Morbidity Borne by Survivors of Acute Myeloid Leukemia Treated With Blood or Marrow Transplantation: The Results of the BMT Survivor Study. J Clin Oncol. 2022 Oct 1;40(28):3278-3288.
- Granroth G, Khera N, Arana Yi C. Progress and Challenges in Survivorship After Acute Myeloid Leukemia in Adults. Curr Hematol Malig Rep. 2022 Sep 19:1–11. doi: 10.1007/s11899-022-00680-6. Epub ahead of print. PMID: 36117228; PMCID: PMC9483315.


