BOSTON—About a third of hematologic cancer patients in a recent cohort study screened positive for executive dysfunction, and more than 17% had memory problems.
The research published in JAMA Oncology pointed out that cognitive dysfunction in these patients had a detrimental effect on cancer survival.
The study team, led by researchers from Brigham and Women’s Hospital and including participation from the VA Boston Healthcare System, conducted the cohort study of 360 patients with blood cancer. A key finding was that impairment in working memory was associated with increased overall mortality (median survival, 10.9 vs. 12.2 months), although impairment in executive function was not.
“Intact cognition is especially important for patients with hematologic or blood cancers because cure is often still possible in advanced disease, and treatment regimens are complex and frequently include inpatient components,” the study authors pointed out. “Moreover, routine treatment regimens and blood transfusion protocols often include drugs that further impair cognition, such as corticosteroids, benzodiazepines, and anticholinergic medications. Finally, all cancer treatment may exacerbate existing health deficits; in a large study of older patients with solid tumors, deaths among the cognitively impaired were most often due to nononcologic causes. Indeed, patients with blood cancer are also at risk of nononcologic causes of death.”
This prospective observational cohort study included all patients 75 years and older who presented for initial consultation in the leukemia, myeloma, or lymphoma clinics of a large tertiary hospital in Boston from Feb. 1, 2015, to March 31, 2017. In an effort to determine the prevalence of domain-specific cognitive impairment and its association with overall survival among older patients with blood cancer, participants underwent screening for frailty and cognitive dysfunction and were followed up for survival.
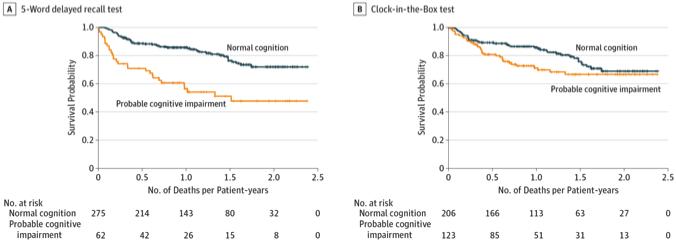
Researchers used the Clock-in-the-Box test to screen for executive dysfunction, while a five-word delayed recall test was used to screen for impairment in working memory. Participants were characterized as robust, prefrail or frail based on the Fried frailty phenotype and Rockwood cumulative deficit model of frailty.
Among 420 consecutive patients approached, 360 agreed to undergo frailty assessment—64.4% male and 35.6% female, mean age 79.8—and 94.7% of them also completed both cognitive screening tests.
Results indicated that 127 patients (35.3%) had probable executive dysfunction on the CIB, and 62 (17.2%) had probable impairment in working memory on the five-word delayed recall. While impairment in either domain was modestly correlated with the Fried frailty phenotype (CIB, ρ = 0.177; delayed recall, ρ = 0.170; P = 0.01 for both), probable cognitive impairment also was present in many phenotypically-robust patients—24 of 104 [23.1%] on CIB and 9 of 104 [8.7%] on delayed recall, the study found.
Overall, patients with impaired working memory had worse median survival (10.9 [SD, 12.9] vs. 12.2 [SD, 14.7] months; log-rank P < 0.001), even when stratified by indolent cancer (log-rank P = 0.01) and aggressive cancer (P < 0.001) and in multivariate analysis when adjusting for age, comorbidities and disease aggressiveness (odds ratio, 0.26; 95% CI, 0.13-0.50).
Participants undergoing intensive treatment were especially affected by impaired working memory and had worse survival (log-rank P < 0.001), the researchers wrote, with that being the only situation in which executive dysfunction also contributed to higher mortality rates (log-rank P = 0.03).
“These data suggest that domains of cognitive dysfunction may be prevalent in older patients with blood cancer and may have differential predictive value for survival,” study authors concluded. “Targeted interventions are needed for this vulnerable patient population.”
1. Hshieh TT, Jung WF, Grande LJ, Chen J, Stone RM, Soiffer RJ, Driver JA, Abel GA. Prevalence of Cognitive Impairment and Association With Survival Among Older Patients With Hematologic Cancers. JAMA Oncol. 2018 May 1;4(5):686-693. doi: 10.1001/jamaoncol.2017.5674. PubMed PMID: 29494732; PubMed Central PMCID:PMC5885202.


