One Clinic Study Showed Effectiveness
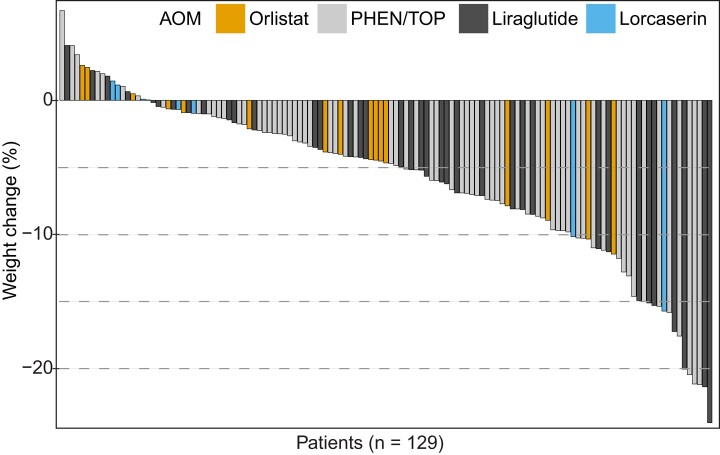
Click to Enlarge: Weight change (%) within the first 15 months among those returning for follow-up visit. Waterfall plot shows individual weight change (%) of patients who returned for follow-up. Each vertical bar depicts one patient, arranged in descending order from maximum weight gain to maximum weight loss, and is colored per initial antiobesity medication prescribed. Source: Journal of the Endocrine Society
AURORA, CO — Antiobesity medications have tended to be underused in the VHA despite a high prevalence of obesity in the veteran population, according to a new study, which added that real-world outcomes reports on use of drugs in veterans also have been limited.
Researchers from the University of Colorado and the Rocky Mountain Regional VAMC, both in Aurora, CO, sought to analyze weight-loss outcomes from a local VHA pharmacotherapy-based weight management clinic (WMC).
The retrospective cohort study of veterans enrolled in a local WMC occurred for 15 months from August 2016 through September 2018 and was followed through November 2019. Patients were offered 1 of 5 available antiobesity medications (AOMs) based on their comorbidities. The researchers assessed any factors associated with weight loss, defined as a 5% or more decrease in weight.
Of 159 patients who were seen in a WMC, 149 (93.7%) of the veterans were prescribed an AOM, and 129 returned for follow-up. Overall, 61/129 (47%) patients achieved 5% or greater weight loss and 28/129 (22%) achieved 10% or greater weight loss within 15 months.
The study, published in the Journal of the Endocrine Society, reported that clinically significant weight loss by percentage over the first 15 months was achieved with phentermine/topiramate ER (-6.3%) and liraglutide (-7.5%) but not with orlistat (-3.9%) and lorcaserin (-3.6%). “Comorbid obstructive sleep apnea was negatively associated with achieving ≥5% weight loss,” the authors pointed out.
“Phentermine/topiramate ER and liraglutide were found to be effective AOMs among veterans,” according to the study. “Further work is needed to mitigate barriers to AOM initiation given the continued rise in obesity.”
The WMC at the VA Eastern Colorado Health Care System began in August 2016 and was started by endocrine clinicians (physicians and nurse practitioners), dieticians associated with VA’s MOVE! weight-loss program and a pharmacist. Veterans were eligible for the clinic if they participated in MOVE! for at least three months, and either had a body mass index (BMI) ≥30 kg/m2 or a BMI ≥27 kg/m2 with at least one weight-related comorbidity.
High Obesity Prevalence
Background information in the article noted that, in 2014, obesity and overweight prevalence among more than 5 million veterans receiving primary care in the VHA was 41% and 37%, respectively. “This prevalence is greater in veterans who receive care at the VHA when compared with those who receive care outside the VHA,” according to the authors, who added, “Alarmingly, 75% of Iraq and Afghanistan war veterans who use the VHA already have overweight or obesity. To address obesity on a wide scale, the VHA has implemented a national evidence-based behavioral weight management program (MOVE!) with a curriculum focusing on diet, exercise, and behavior change. However, participation rates are low, and weight loss in participants is just 2.2% of body weight after 3 years.”
The researchers suggested that one potential way to enhance weight loss success among veterans is the wider adoption of antiobesity pharmacotherapy as an adjunct to behavioral weight management. They advised that the strategy is supported by many professional society guidelines including the nVHA/Department of Defense, Endocrine Society, American Heart Association, American College of Cardiology and The Obesity Society.
“Despite the availability of antiobesity medications (AOMs) on the VHA’s national formulary, utilization of these medications through 2019 was very low with only 1.1% of eligible veterans receiving an AOM prescription within 1 year of MOVE! enrollment,” the authors wrote. “AOMs remain largely underused in the VHA because of various prescription barriers, including restrictive criteria for use and approval and follow-up processes.”
The study added that the use of semaglutide, a once-weekly glucagon-like peptide-1 receptor agonist that is popular because of its ability to produce a greater magnitude of weight loss than previously available medications, is limited by medication shortages and national guidelines that restrict it as first-line therapy only for a subpopulation of patients who qualify for AOMs based on standard Food and Drug Administration criteria for AOM use.
- Ni K, Rogowitz E, Farahmand AK, Kaizer LK, Arbet J, Cunningham CR, Thomas EA, Saxon DR. Weight Loss Outcomes in a Veterans Affairs Pharmacotherapy-based Weight Management Clinic. J Endocr Soc. 2024 Mar 6;8(5):bvae042. doi: 10.1210/jendso/bvae042. PMID: 38515583; PMCID: PMC10957131.


