Feature Could Help Explain Sleep, Pain Issues
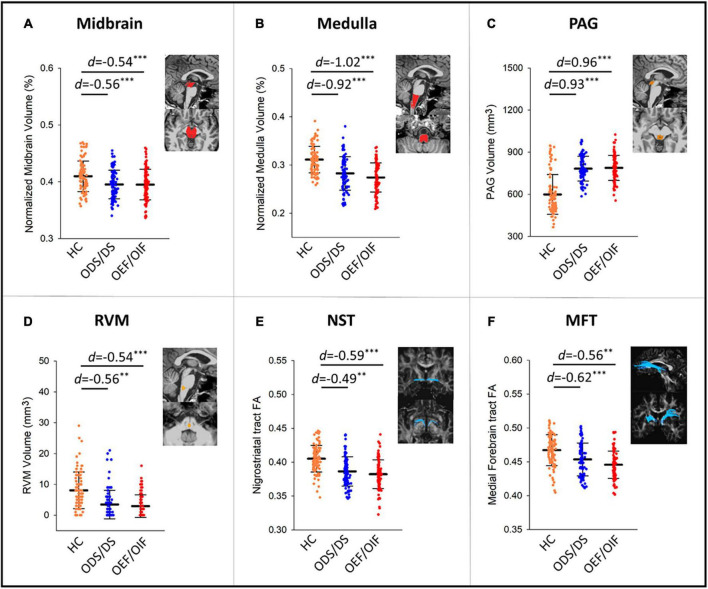
Click to Enlarge: Group comparisons in volume measures in the midbrain (A), medulla (B), PAG (C), RVM (D), and FA measures within NST (E), and MFT (F) tracts. PAG, periaqueductal gray; RVM, rostral ventromedial medulla; DLF, dorsal longitudinal fasciculus; NST, nigrostriatal tract; MFT, medial forebrain tract; TPT, temporopontine tract; FA, fractional anisotropy; HC, healthy control; d, Cohen’s D effect size. Significant levels: **0.001 ≤ p < 0.01, ***p < 0.001. Source: Frontiers in Molecular Neuroscience
PALO ALTO, CA — Gulf War and Iraq/Afghanistan veterans have significantly smaller brainstem volumes compared to healthy civilians, and damage to the brainstem structure of these veterans could potentially lead to sleep disturbances and chronic pain, according to a recent study.
The study, published earlier this year in Frontiers in Molecular Neuroscience, investigated whether Gulf War and Iraq/Afghanistan veterans “present similar brainstem damage and whether these brainstem structural differences are associated with major symptoms as in Gulf War Illness (GWI), a type of chronic multisymptom illness,” the study reported.1
The study authors are affiliated with the VA Palo Alto Health Care System in Palo Alto, CA, and Stanford University School of Medicine in Stanford, CA.
In the study, the authors used “structural magnetic resonance imaging and diffusion tensor imaging to measure the volumes of subcortices, brainstem subregions and white matter integrity of brainstem fiber tracts in 188 veterans, including 98 Persian Gulf War veterans and 90 Iraq/Afghanistan veterans,” the study authors wrote. “All veteran data were collected at the War Related Illness and Injury Study Center (WRIISC) at VA Palo Alto Health Care System.”
The research team sought to explore this topic, because “about one-third of veterans who served in the Gulf War (as well as Iraq/Afghanistan) have developed unexplained symptom constellations involving multiple systems, referred to as Chronic Multisymptom Illness (CMI).”
The authors pointed out that the “causes and pathological mechanisms underlying CMI remain unknown, and since the brainstem is known as a central control of sleep-awake cycle and a central control of pain inhibition,” they wanted to learn more about the neuropathological basis underlying CMI.
“Through analyses of MRI imaging, we found that compared to age-matched healthy civilians from public data repositories, veterans who served for both campaigns (Operation Desert Shield/Desert Storm [ODS/DS] and Operation Enduring Freedom/Operation Iraqi Freedom [OEF/OIF]) presented with substantially smaller brainstem volume,” lead author Yu Zhang, MD, PhD, a research specialist at VA Palo Alto Health Care System, told U.S. Medicine.
In addition, the authors found that, in veterans deployed during the 1990-91 Persian Gulf War, “structural deficits in brainstem volume, fibers and nuclei that participate in sleep-awake regulation are associated with severe sleep disturbances,” Zhang suggested. Also, “structural deficits in brainstem fibers and nuclei that participate in pain regulation are associated with greater pain perception in these veterans,” she added, noting, “We consider that the brainstem structure is vulnerable and may be damaged during/after the Gulf War, potentially leading to sleep disturbances and chronic pain.”
The research team observed that “brainstem volumes of these soldiers (who presented with CMI) are smaller than those of age- and sex-matched healthy civilians who have no complaint of sleep/pain or other neurological issues,” Zhang explained. Because this was an observational study that analyzed data from a population at a single point in time, the authors can’t demonstrate how the brainstem damage and smaller brainstem volumes occurred in the military personnel, Zhang wrote in an email.
The authors suggest that “evidence from this study and other research groups seem to point to brainstem damage as a crucial part of CMI/GWI pathology,” Zhang added.
Different Physiopathologic Mechanism
The study notes, however, that although brainstem structural deficits are significantly correlated with increased sleep difficulties and pain intensities in Gulf War veterans, “this effect wasn’t observed in veterans deployed to Iraq/Afghanistan, which suggests different physiopathologic mechanisms underlying veterans of each group.”
One key concern leading to these observations might be the “different combat-time and age between the two groups,” the authors suggested. In addition, “combat/environmental exposures, uses of anti-nerve gas agents and multiple vaccinations could also be influencing factors,” they said.
The authors advised that “further investigations are valuable to reveal the biological basis of the different imaging-symptom relationships in Gulf War and Iraq/Afghanistan veterans.”
For veterans who present with CMI (mainly suffering from fatigue, sleep or pain issues), the authors recommended that clinicians to “consider treatment stimulating the brainstem (e.g., vagus nerve stimulation) and dietary neurotransmitters that support brainstem regulation,” Zhang said.
This study’s findings “provide important implications for future clinical care and treatment development,” according to the authors. “Understanding the neuroimaging and neuropathological relationships in Gulf War and Iraq/Afghanistan veterans may improve clinical management and treatment strategies for modern war-related chronic multisymptom illness,” the authors explained.
Limitations of the study include that it lacked a healthy veterans control group and instead used healthy civilians from public data sources, the study reported. As a result, “the findings from group comparisons could potentially reflect a limited characterization of GWI, which is considered a post-deployment illness due to exposures to neurotoxic circumstances,” the authors suggested. Also, the study didn’t have “comprehensive clinical information available for the healthy controls, which could limit how specific this study could be in examining the influences of these conditions,” they added.
Another limitation is the study “only focused on investigating sleep and pain related brainstem alterations, though other conditions such as chronic fatigue, pulmonary, gastrointestinal problems and neurological conditions (e.g., headache, impaired memory and concentration) may have a significant impact on brainstem structures,” the researchers pointed out.
In future studies, the authors said they will include assessment of cognitive batteries in ongoing strategies because “further investigations of the relationship between brainstem structures and other symptom domains (e.g., fatigue, autonomic and neurocognitive status) in Gulf War veterans will be needed.”
- Zhang Y, Moore M, Jennings JS, Clark JD, Bayley PJ, Ashford JW, Furst AJ. The role of the brainstem in sleep disturbances and chronic pain of Gulf War and Iraq/Afghanistan veterans. Front Mol Neurosci. 2024 Jan 8;16:1266408. doi: 10.3389/fnmol.2023.1266408. PMID: 38260809; PMCID: PMC10800562.

